Abstract
Introduction: Vitamin D has immunomodulatory effects and vitamin D deficiency has been associated with autoimmune responses and increased risk of infections. Vitamin D-mediated antimicrobial and anti-inflammatory responses play an effective role in the prevention of various respiratory tract infections including coronavirus disease 2019 (COVID-19). Aims and objective: To evaluate the therapeutic role of vitamin D via immunomodulation in COVID-19 through a Knowledge, Attitudes and Practices (KAP) study of pan India healthcare practitioners (HCPs) to arrive at a common consensus statement regarding dosage and duration of vitamin D for immune-modulatory function. Methods: A pan-India, online, questionnaire-based, KAP survey was conducted on vitamin D and its role in immunomodulation in COVID-19 from April 2021 to January 2022 followed by polling obtained from 2,338 HCPs through round table meetings (RTMs). Results: Approximately 64% of HCPs considered the use of vitamin D in COVID-19 patients for various reasons including prevention of illness, reduced ICU stay, reduction in morbidity and mortality along with decrease in the levels of inflammatory markers in COVID-19 patients. For the dosage regime, 47% of HCPs preferred vitamin D 60,000 IU
weekly while 45% of HCPs preferred both 60,000 IU weekly and 2,000 IU daily dose for boosting immune system in their patients. Conclusion: The panel agreed that vitamin D levels of 40 ng/mL and above appear to confer better immune-protective response to several infections including COVID-19.
Keywords: Vitamin D, COVID-19, healthcare practitioners, immunomodulation
Vitamin D, also referred to as the “sunshine vitamin” plays a major role in calcium absorption and bone mineralization.1 It has immunomodulatory effects and vitamin D deficiency has been associated with autoimmune responses and
increased risk of infections.1,2 The beneficial effects of vitamin D are realized primarily based on its role in innate antimicrobial immune response pathways.3 Vitamin D-mediated antimicrobial and anti-inflammatory responses play an effective role in the prevention of various respiratory tract infections (RTIs).4 In recent times, there is a surge of evidence regarding the role of vitamin D in cardiometabolic outcomes.5 Serum 25-hydroxyvitamin D [25(OH)D] levels are inversely correlated with upper RTIs.6
Despite this awareness, vitamin D deficiency is highly prevalent among the population of India. Irrespective of the age group or existence of prevailing health conditions, the prevalence of vitamin D deficiency ranges from 40% to 99%, with most studies reporting a prevalence of 80-90%.7 During the ongoing COVID-19 pandemic, when there were no immunizations available, there was an urgent need to keep the population healthy and devoid of major deficiencies that could have implications on immunity. Even when vaccines are available, it is necessary to continue to build immunity and to reduce the deficiencies that could adversely affect immunity.
Vitamin D plays a vital role in regulation of cytokine storm due to immunomodulatory function. Invasion of viral or other respiratory pathogens activates innate immune response resulting in increased local production of 1,25-dihydroxyvitamin D [1,25(OH)2D].8 Downstream events involving CYP27B1 and vitamin D
receptors either constitutively expressed by airway epithelia or inductively expressed by pulmonary alveolar macrophages, lead to viral neutralization and clearance of viral load. The positive effects of vitamin D supplementation in COVID-19 infections include faster viral clearance, immunomodulation, reduced severity and mortality of the disease.9 Also, the recommendations for dosages and duration for use of vitamin D by different bodies vary and there is a lack of consensus statement for use of vitamin D for immune-protection.
Hence, this study was designed with the objective to achieve a common consensus statement on the therapeutic role of vitamin D for immunomodulation in COVID-19 via Knowledge, Attitudes and Practices (KAP) study of the healthcare practitioners (HCPs).
Methods
A pan-India, online, questionnaire-based survey was conducted on vitamin D and its role in immunomodulation in COVID-19 from April 2021 to January 2022, based on an initial discussion with an expert panel of endocrinologists from across the country, to evaluate the awareness of HCPs in India regarding the role of vitamin D supplementation in COVID-19. The questionnaire-based survey was conducted online through email. After the online survey of HCPs,
26 virtual regional round table meetings (RTMs) were conducted in various locations across India. The survey questionnaires were again rolled in the virtual RTMs and online polling was conducted to gather the opinions of the HCPs.
RESULTS
A total of 2,338 HCPs participated in the study, which included Consultant Physicians, Diabetologist, Endocrinologists and Cardiologists.
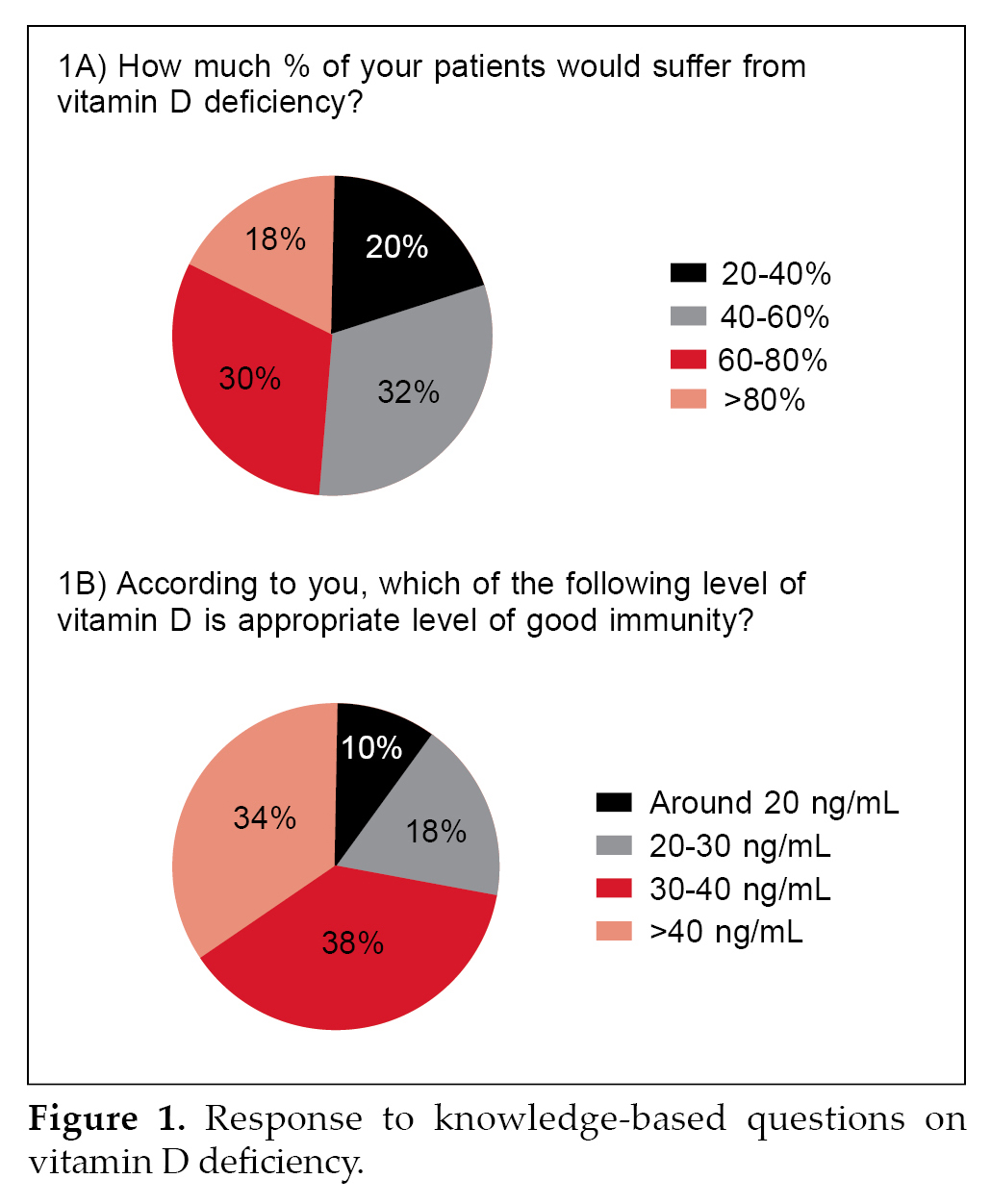
HCPs response to the prevailing population-centric view of vitamin D deficiency was variable. About 30% of HCPs were of the opinion that 60-80% of the patients have vitamin D deficiency while according to 32% of HCPs, 40-60% of the patients have vitamin D deficiency (Fig. 1A).
About 38% of the HCPs responded to a vitamin D level of 30-40 ng/mL as appropriate for maintaining good immunity, while 34% of HCPs were of the opinion that >40 ng/mL was the appropriate level (Fig. 1B).
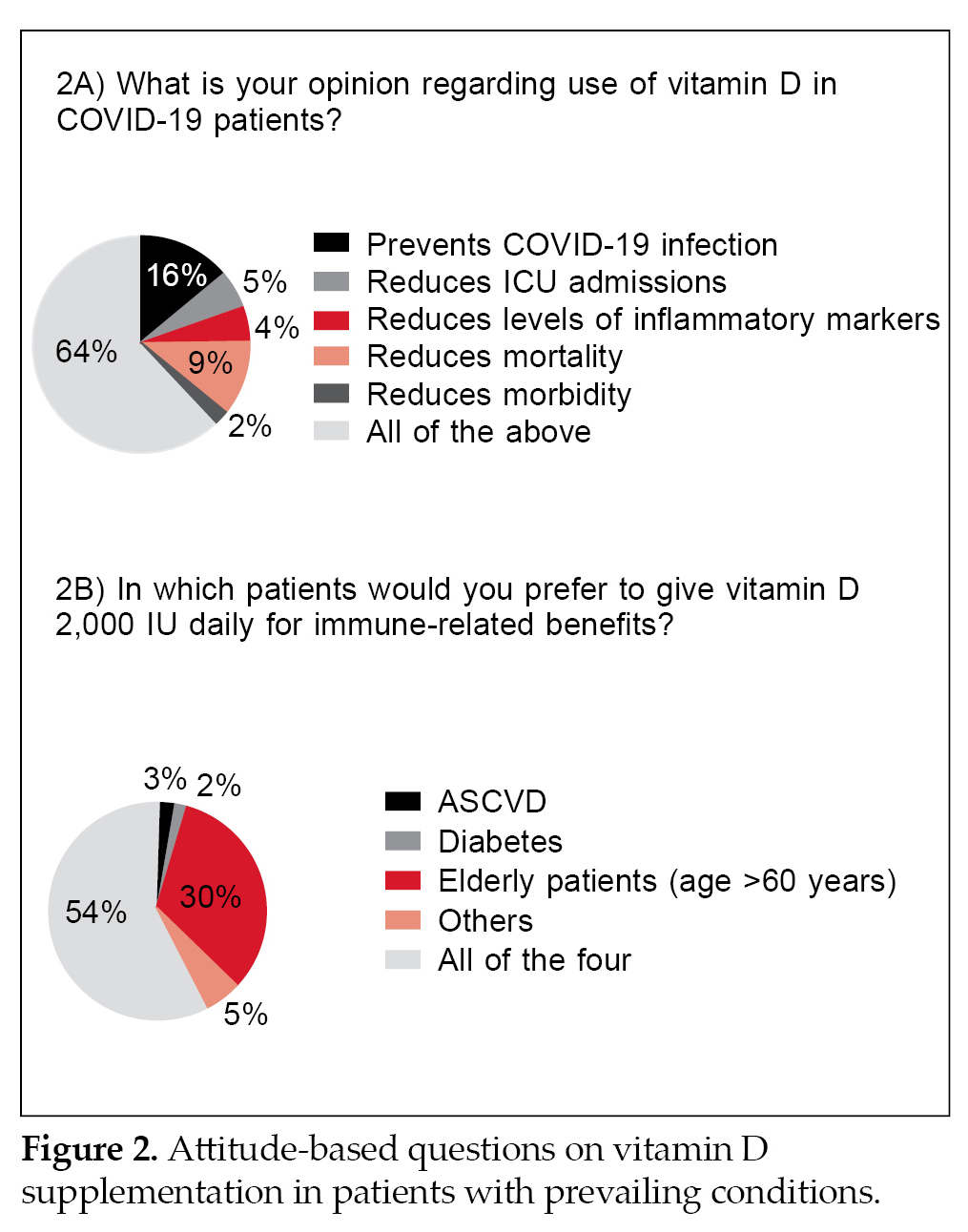
Almost 64% of HCPs considered the use of vitamin D in COVID-19 patients for various reasons including prevention of illness, reduced ICU stay, reduction in morbidity and mortality along with decrease in the levels of inflammatory markers (Fig. 2A). About 54% of the HCPs said that they would consider prescribing 2,000 IU daily dose of vitamin D in elderly patients
(>60 years) and those with atherosclerotic cardiovascular disease (ASCVD), diabetes, hypertension, chronic respiratory diseases and chronic liver diseases (Fig. 2B).
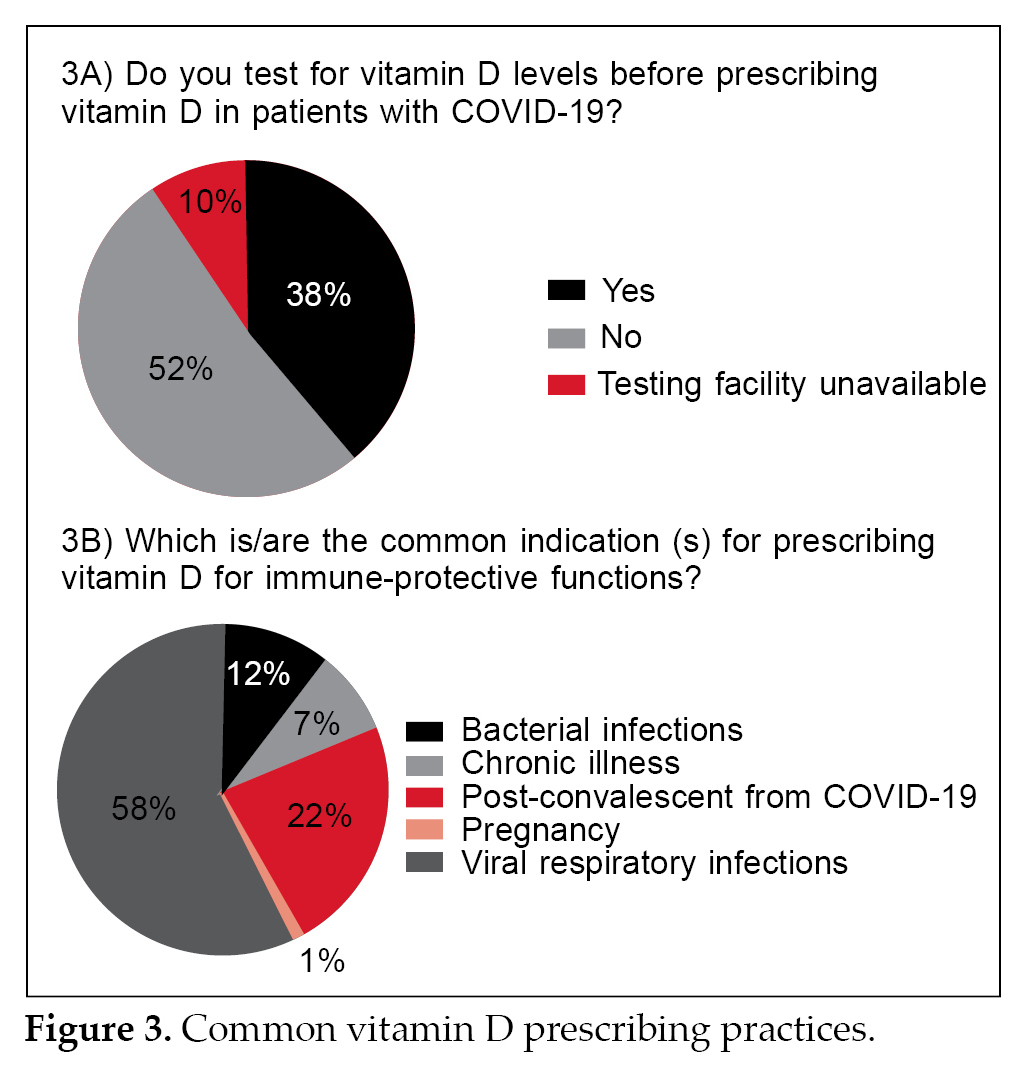
With regard to questions pertaining to vitamin D supplementation in COVID-19 affected individuals, 52% of the HCPs preferred not to test for vitamin D levels before prescribing it (Fig. 3A). Approximately 58% of HCPs prescribed vitamin D for viral respiratory infections, while 22% of HCPs prescribed vitamin D in post-COVID-19 convalescent patients (Fig. 3B).
Regarding dosage regime, 47% of HCPs preferred vitamin D 60,000 IU weekly, while 45% preferred both vitamin D 60,000 IU weekly and 2,000 IU daily for boosting the immune system in their patients (Fig. 4A).
Seventy-two percent of HCPs prescribed vitamin D
for 8 to 12 weeks, while 15% of HCPs considered giving vitamin D for over a period of 6 months to 1 year (Fig. 4B).
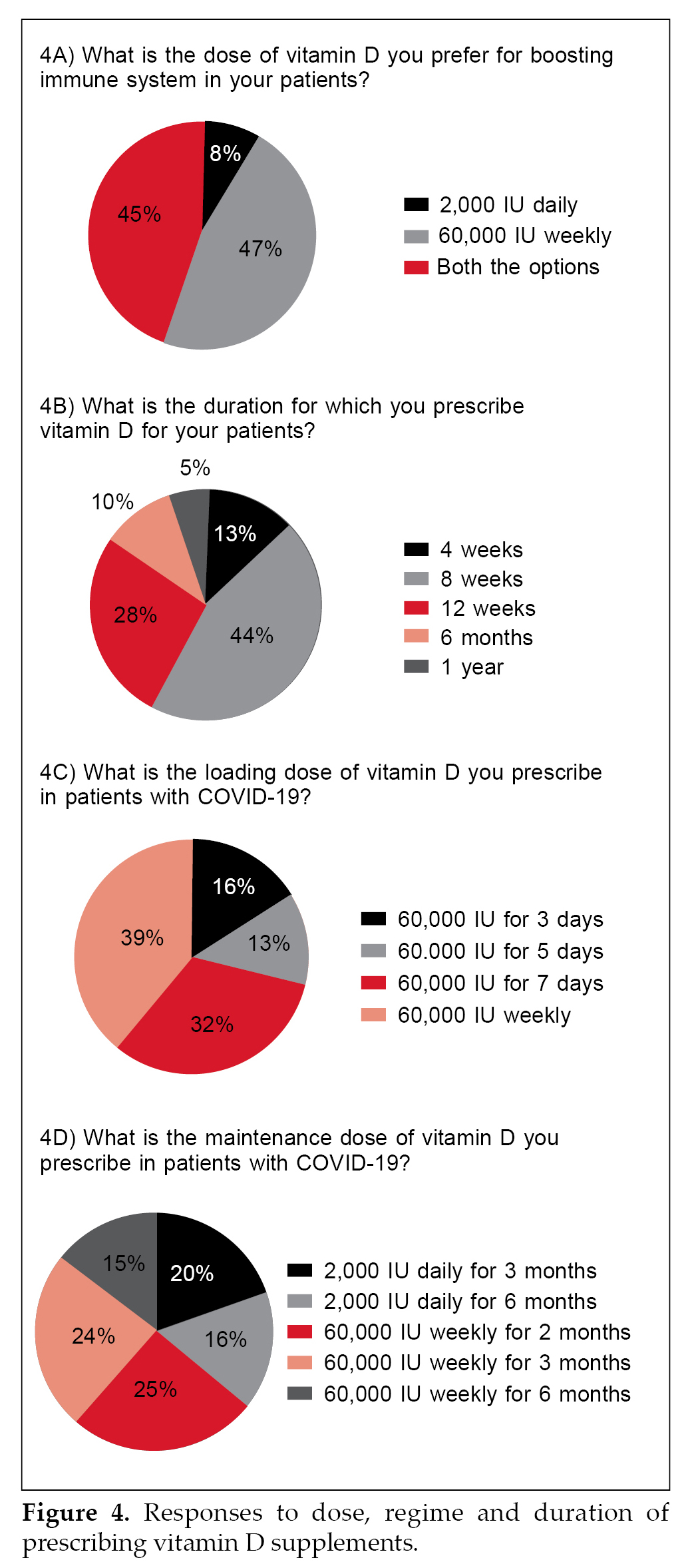
Regarding loading dose of vitamin D in COVID-19, vitamin D 60,000 IU daily for 5 to 7 days was the preferred dose of 45% of HCPs, while 39% HCPs preferred a weekly regime of 60,000 IU of vitamin D
(Fig. 4C). Sixty-four percent of HCPs prescribed vitamin D 60,000 IU weekly for 2 to 6 months as maintenance dose in COVID-19 patients, while 36% of HCPs switched to 2,000 IU daily for 3 to 6 months as maintenance dose (Fig. 4D).
DISCUSSION
The results obtained from the survey and polling from RTMs indicate that there is a high awareness among the HCPs about the prevalence of vitamin D deficiency and supplementation of vitamin D for boosting immunity. But responses with regard to dosage regime, loading and maintenance dosages of vitamin D in COVID-19 were variable.
Despite the increasing awareness of the role of vitamin D
in bone health, cardiovascular metabolism and immunity, a significant proportion of Indian population is vitamin D
deficient. It is highly pertinent for HCPs to recognize the need for vitamin D supplementation and to ensure its use inadequate doses (loading and maintenance dose) for the recommended duration. This need is much more enhanced in the current COVID-19 pandemic times where strategies that help boost immunity and reduce morbidity and mortality with minimal side effects are much warranted.
Individuals with low vitamin D levels (<30 ng/mL) seem to be more prone for upper RTIs.7 Opinion regarding the cut-off level was divided in our survey. While 38% of HCPs were of the opinion that vitamin D
level of 30-40 ng/mL was sufficient for maintaining a good immunity, 34% opined that levels >40 ng/mL
were adequate. Most of the HCPs (52%) in our survey favored supplementing vitamin D in patients with COVID-19 without prior checking vitamin D levels. This could have been due to the poorly defined reference estimates, variations among standard tests10 or lack of testing facilities.
Currently, there is no consensus on the dose of vitamin D
to be used for either prevention or treatment of COVID-19. Instead, what most experts recommend is vitamin D supplementation for which several strategies have been proposed.
Rastogi et al evaluated the positive effects of vitamin D
supplementation in asymptomatic and mildly symptomatic COVID-19 patients. Participants were randomized to receive daily 60,000 IU of cholecalciferol for 7 days with therapeutic target 25(OH)D >50 ng/mL
(intervention group) or placebo (control group). It was found that daily cholecalciferol 60,000 IU supplementation was useful for achieving vitamin D
level >50 ng/mL in 75% of patients by 14th day. Therapeutic high-dose cholecalciferol led to severe acute respiratory coronavirus 2 (SARS-CoV-2) RNA negative in additional 41.7% participants (p < 0.001) and was useful for SARS-CoV2 RNA clearance.11
In another study by Harinarayan et al, administration of 60,000 IU of vitamin D3 once a week with daily 1,000 IU (along with calcium 1 g/day) for 8 weeks was done to attain a vitamin D level of 30 ng/mL in deficient patients. After 2 months, about one-fourth of the patients attained vitamin D sufficiency. With continued dosage of 60,000 IU of vitamin D3 every 2 weeks with 1,000 IU daily (along with calcium
1 g/day), 46% of the patients attained vitamin D sufficiency by the 5th month.12 In an open-label, randomized, prospective study of 10 weeks effect of oral high-dose vitamin D regimens (60,000 IU weekly) and daily low-dose of vitamin D regimen of 1,000 IU were evaluated in vitamin D deficient patients (serum levels <30 ng/mL). The study concluded that high-dose vitamin D (60,000 IU weekly) regimen rapidly normalized 25(OH)D levels and ensure symptomatic relief earlier than daily dosing of 1,000 IU vitamin D for same duration.13 The various dosage regimens and duration of vitamin D used in these studies indicate the need for a common consensus statement for the HCPs.
CONCLUSION
Overall, majority of HCPs surveyed acknowledged the prevalence of vitamin D deficiency in general population and also recognized the immune boosting potential of vitamin D, especially in COVID-19-infected individuals. The results of the online survey and RTMs suggest that vitamin D may have potential role in decreasing morbidity, mortality and ICU admission in COVID-19 patients through regulation of cytokine storm via immunomodulatory actions. Maintenance of optimal vitamin D levels (≥40 ng/mL) appears to confer better immune-protective response to several infections including COVID-19. Most of the HCPs recommended vitamin D supplementation of 60,000 IU/week for 2 to 6 months and 2,000 IU/day for 3 to 6 months in vitamin D-
deficient patients for optimal response to therapy in COVID-19 patients. The immunomodulatory function of vitamin D should be further explored considering the increased awareness and use of vitamin D for immune protection from this KAP study.
Acknowledgments
The Endocrinologist panel would like to acknowledge Dr Mahesh Abhyankar, Dr Ashish Prasad, Dr Santosh D Kale from Scientific Services of USV Pvt Ltd, Mumbai, Maharashtra, India for the study analysis support.
Financial Support
This study was funded by USV Pvt Ltd, Mumbai, Maharashtra, India.
References
- Laird E, Ward M, McSorley E, Strain JJ, Wallace J. Vitamin D
and bone health: potential mechanisms. Nutrients. 2010;2(7):693-724.
- Aranow C. Vitamin D and the immune system. J Investig Med. 2011;59(6):881-6.
- Liu PT, Stenger S, Li H, Wenzel L, Tan BH, Krutzik SR, et al. Toll-like receptor triggering of a vitamin D-
mediated human antimicrobial response. Science. 2006;311(5768):1770-3.
- Gombart AF. The vitamin D-antimicrobial peptide pathway and its role in protection against infection. Future Microbiol. 2009;4(9):1151-65.
- Sacheck JM, Huang Q, Van Rompay MI, Chomitz VR,
Economos CD, Eliasziw M, et al. Vitamin D supplementation and cardiometabolic risk factors among diverse schoolchildren: a randomized clinical trial. Am J Clin Nutr. 2022;115(1):73-82.
- Ginde AA, Mansbach JM, Camargo CA Jr. Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2009;169(4):384-90.
- Aparna P, Muthathal S, Nongkynrih B, Gupta SK. Vitamin D deficiency in India. J Family Med Prim Care. 2018;7(2):324-30.
- Peng MY, Liu WC, Zheng JQ, Lu CL, Hou YC, Zheng CM, et al. Immunological aspects of SARS-CoV-2 infection and the putative beneficial role of vitamin-D. Int J Mol Sci. 2021;22(10):5251.
- Pinheiro MM, Fabbri A, Infante M. Cytokine storm modulation in COVID-19: a proposed role for vitamin D
and DPP-4 inhibitor combination therapy (VIDPP-4i). Immunotherapy. 2021;13(9):753-65.
- Amrein K, Scherkl M, Hoffmann M, Neuwersch-Sommeregger S, Köstenberger M, Tmava Berisha A, et al. Vitamin D deficiency 2.0: an update on the current status orldwide. Eur J Clin Nutr. 2020;74(11):1498-513.
- Rastogi A, Bhansali A, Khare N, Suri V, Yaddanapudi N,
Sachdeva N, et al. Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomized, placebo-controlled, study (SHADE study). Postgrad Med J.
2022;98:87-90.
- Harinarayan CV, Appicatlaa L, Nalini BA, Joshi S. Efficacy and safety of cholecalciferol supplementation in vitamin D
deficient subjects based on endocrine society clinical practice guidelines. Endocrinol Metabol Syndrome. 2012;S4:004.
- Singh V, Misra AK, Singh M, Midha NK, Kumar B, Ambwani S, et al. An open-label, randomized, 10 weeks prospective study on the efficacy of vitamin D (daily low dose and weekly high dose) in vitamin D deficient patients. J Family Med Prim Care. 2019;8(6):1958-63.