Published in IJCP
January-March 2023
Review Article
Transition Care in Type 1 Diabetes. Five Questions and Five Principles
May 01, 2023 | Simrita Chawla, Jubbin Jagan Jacob
Diabetes & Endocrinology
Abstract
Management of type 1 diabetes mellitus during the period of adolescence to young adulthood is among the most challenging in the field of diabetes care. At around the age of 18 there is a physical transfer of care from pediatric physicians to adult physicians. Alongside there is transfer of responsibility of self-care from parents to the patient over a period of time. Unique medical problems encountered in this age group include puberty induced increase in insulin requirements, an increase in psychiatric comorbidities including substance use and abuse, disconnect with health care teams, and problems related to reproductive care and contraception. This is reflected in the poorer outcomes seen in this age group including an increase in acute complications, increase in hospitalizations with diabetic emergencies, poor glucose control and an increase in loss to follow. The poor metabolic control during this period leads to establishment of early chronic macro and microvascular complications. A structured transition care is a planned purposeful process that address these unique medical, psychological, and vocational needs among these patients that smoothens out the process of transfer to adult care teams. The models that have been proven to be useful in improving outcomes include the use of separate transition clinics, use of transition coordinators and enrollment into young patients support groups. Regardless of the model used there are five overarching principles that define this process of transition care. They can be summarized in five Cs which include: appropriate communication, assessment of self-care needs, building competence, using collaborative teams, and finally providing care and counseling for psychological issues.
Keywords: Transition care, type 1 diabetes mellitus, adolescence, young adults, transfer of cares
Introduction
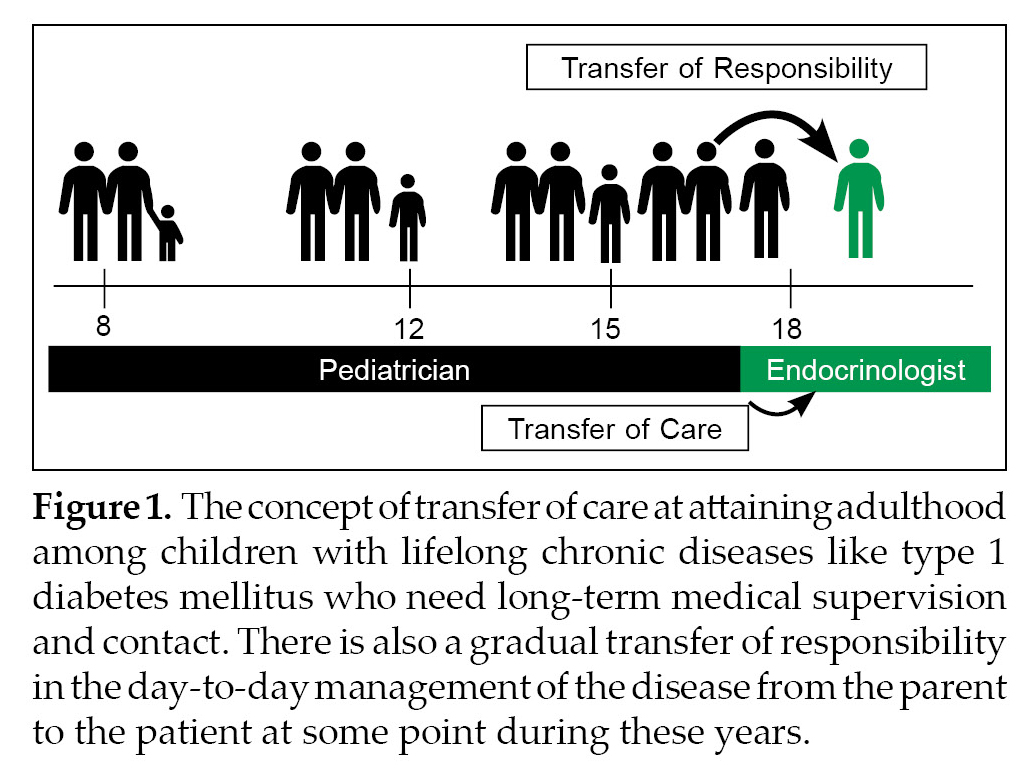
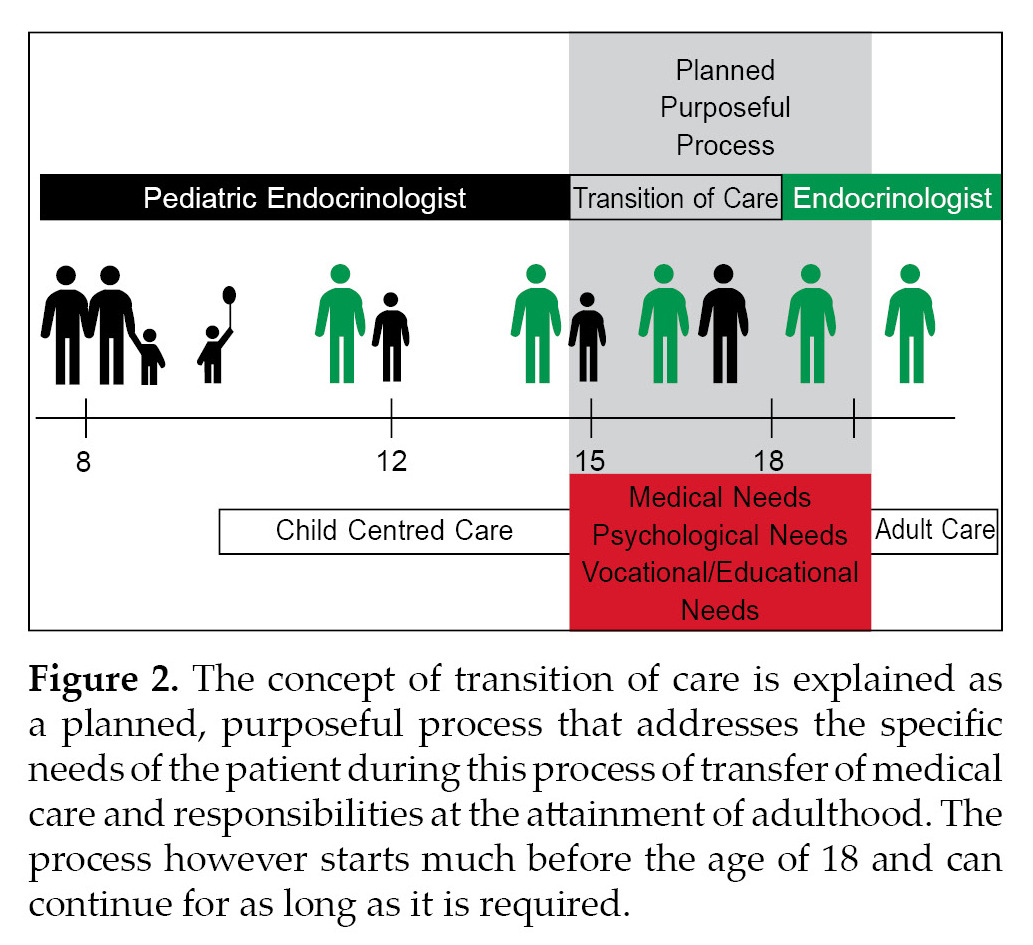
Diabetes management in our country is a challenging task regardless of the type of diabetes mellitus or associated comorbidities and complications. Among the many complicated patients that are encountered in a diabetic clinic the most challenging in our opinion is the management of type 1 diabetes mellitus (T1DM) during adolescence and early young adult- hood. During this period young patients may encounter a transfer of care from a pediatric endocrinologist to an adult endocrinologist and a transfer of responsibility of day-to-day diabetes care from parents to self (Fig. 1). Additionally, some children may also encounter the need to adjust to a new living situation away from the support of family and friends in a new city as they leave for college, further training, employment, or marriage. Transition of care is distinct from transfer of care among adolescents with T1DM in that it is defined as “a planned purposeful process that specifically addresses the unique medical, psychological, social, vocational and educational needs of these children as they move from pediatric to adult care for chronic lifelong diseases like T1DM” (Fig. 2).1
Q1. Why is Transition Care Needed?
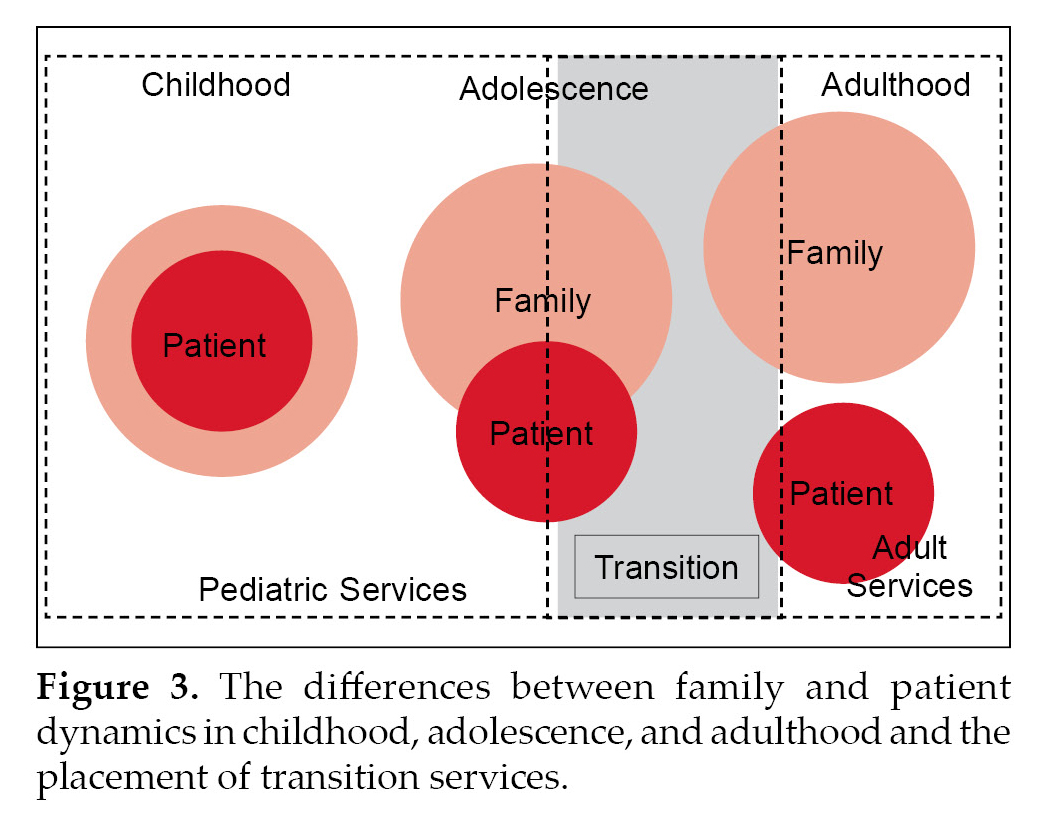
A child or an adolescent diagnosed with a chronic disorder like T1DM must carry the disease into his/her adulthood and beyond. The primary goal of transition care is to help the child with T1DM to seamlessly shift from a pediatric family centred diabetes care environment to an independent adulthood (Fig. 3). There are several reasons why transition care is essential. These include:
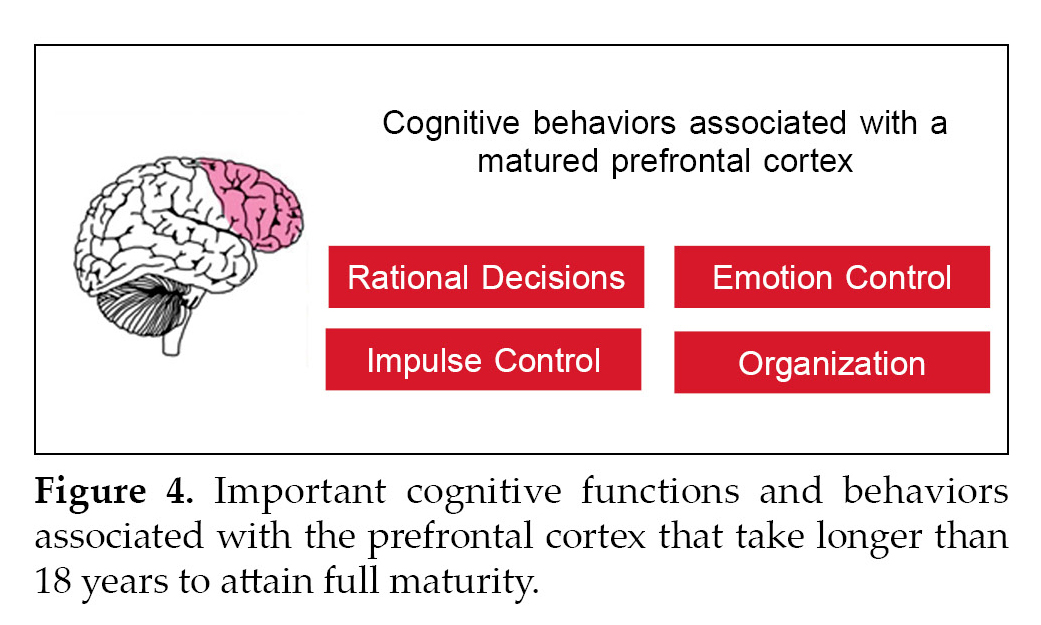
- Underdeveloped prefrontal cortex in young adults. Though crossing the age of 18 is considered the threshold of adulthood in most countries it is slowly being realized that complete maturity of the prefrontal cortex only happens in the early twenties.2 The prefrontal cortex is an area responsible for many of the important cognitive behaviors that are associated with adulthood (Fig. 4).
- Insulin resistance related to pubertal hormone changes. Puberty induces a combination of hormonal changes involving the gonadal and growth axis that leads to an increase in insulin resistance. Normal children in late puberty secrete almost double the amount of insulin compared to children in early puberty. In adolescents with T1DM this corresponds to an increased requirement of exogenous insulin and difficulty in achieving glucose targets. Additionally, puberty may unmask dawn phenomenon in many adolescents and girls may note an increase in insulin requirements in the premenstrual period.3,4.
- An increase in psychological issues during this period. Almost all adolescents struggle during this period where they are developing their identity and autonomy independent of the family. Adolescents with T1DM have to face additional challenges including adhering to insulin and self-monitoring regimes, uncomfortable interactions with peers, classmates and colleagues at work, disagreements with family regarding diabetes self-care, fear of short-term complications like hypoglycemia and hospitalizations and fear of long-term complications and feelings of guilt when glucose control is suboptimal.5 All these lead to an increase in the prevalence of anxiety disorders, panic attacks and psychological distress.6 Depression and depressive symptoms are common among T1DM in this age group. In the SEARCH study girls with T1DM had a 10.9% prevalence of moderate to severe depressive symptoms.7 Eating disorders are 2.4-fold more common among girls with T1DM compared to girls without diabetes of similar age.8
- Sexual and reproductive health issues. There is no reason for adolescents and young adults with T1DM to behave any differently from their
peers without diabetes. All young patients should receive preconceptional counseling and be given appropriate contraception advice.
- Alcohol, smoking and drug use. Again, there is no evidence that alcohol, tobacco, and drug use rates are any different among adolescents with T1DM compared to peers who do not have diabetes. Alcohol worsens hyperglycemia immediately and increases the risk for delayed hypoglycemia. All though abstaining from alcohol is the safest response, in practical terms, young people with T1DM need to be educated about safe drinking and decreasing any risks by maintaining hydration, eating adequate carbohydrates, reducing insulin doses if required, and monitoring blood glucose levels.
- Social, educational, and vocational changes. Adolescents during the transition period have major changes in their life that includes going for undergraduate or postgraduate studies on occasions to cities far from where they have been brought up in, independent living in hostels and other student accommodations with difficult access to appropriate diets and meals, earning for their livelihood, training and internship which may include shift and night duties and in a small number of cases getting married and starting a family of their own.
Q2. Are Bad Outcomes Noted in the Transition Period?
As noted above, the period of transition is potentially associated with the interruption of a long-term “comfortable” relationship with health care providers especially at a time when the adolescent is confronting multiple issues related to changing metabolism and the development of identity and autonomy. Poor health choices with smoking, alcohol use especially binge drinking, and loss of parental supervision of diet and insulin administration may complicate matters further. The poor outcomes noted during this period include:
- Poor metabolic control. Current hemoglobin A1c (HbA1c) targets from the American Diabetes Association (ADA) for children between the ages of 13 years and 18 years is <7.5% (58.5 mmol/moL) and after the age of 19 years is <7% (53 mmol/moL).9 Most teenagers and young adults struggle to meet these targets. Data from the SEARCH Study in youth with T1DM suggests that only 32% of teenagers (13 to 18 years) and 18% of the young adults (19 onwards) achieved these targets.10 This stands in contrast with 56% of adults achieving HbA1c targets of <7% (53 mmol/moL).11
- Loss to follow-up. Transitioning older teenagers and young women are at particularly high-risk of disengagement from health care providers because of the competing distractions. Though there is limited published information about the frequency of contact between young people and health care professionals. Clinic attendance was significantly lower (8.5 ± 2.3/years vs. 6.7 ± 3.2/years) over 3 years when teenagers were transitioned from pediatric to adult services in Germany when compared to previous attendance at pediatric clinics.12
- Risk of acute complications. A large cohort of 1,243 children (aged from infancy to 19 years) was followed up for 3,994 person-years in Denver. The primary outcome in the study was the rate of acute presentation to emergency department with ketoacidosis and severe hypoglycemia. The overall incidence of diabetic ketoacidosis was 8 episodes/100 person-years in the cohort. The highest incidence of diabetic ketoacidosis was seen among adolescent between the ages of 13 years and 19 years with rates over 12 episodes/100 person-years.13 Another study from Ontario looked at 1,507 patients with type 1 diabetes followed for 4 years after transition to adult clinic. The hospitalization rates increased from 7.6 episodes/100 patient-years prior to transition to 9.5 admissions/100 patient-years after transition (p = 0.03).14
- Emergence of chronic complications of diabetes. Chronic complications related to diabetes are extremely rare among preadolescents. Even among adolescents, clinically apparent diabetes related complications are very rare. Although preclinical evidence of diabetes related microvascular complications maybe present in adolescents. Evidence of early atherosclerotic processes including fatty streaks and intimal lesions are seen in autopsy studies conducted on adolescents and young adults.15
- Premature mortality during transition. Mortality rates are increased in patients with diabetes compared to the general population at all ages. Within this cohort of patients with diabetes mellitus, men have an increased risk of death compared to women at all age groups except between the ages of 5 years and 15 years. However, the relative risk (RR) of death is much higher in women at all ages. The RR of death (standardized mortality ratio [SMR]) is 4 for women and 2.7 for men. The peak SMR in women was between the ages of 20 years and 29 years at which point it was as high as 5.7. Most of this information has come from a very large cohort of patient with insulin treated diabetes from the United Kingdom.16
Q3. What Are the Current Transition Models That Have Been Shown to Work?
Currently, there are no randomized controlled trials examining the overall efficacy of a structured transition program among adolescents and young adults. However, structured transitional care has been demonstrated in cohort studies to have better outcomes in terms of less loss to follow-up, better HbA1c levels, fewer admissions with diabetic ketoacidosis, and fewer long-term complications at the end of the transition.17,18 There are three basic models which can be followed which have been found to improve outcomes.
- Dedicated transition or young adult clinics. The earliest and simplest model appears to be a dedicated transition clinic staffed by both pediatric and adult diabetes teams which handle children in transition for a given period prior to complete transfer of care to the adult diabetes services. Logan et al. from the United Kingdom reported data from a structured intervention that consisted of a year-long transition clinic which comprised of both pediatric and adult physicians and nurses. Patients were seen three times a year and on two out of the three occasions, the patient could choose the provider they wished to see (doctor, nurse, dietician, or clinical psychologist). Over a period of 3 year, patients had an 84% attendance rate, a drop of HbA1c from 9.7% to 9.0% (first to last visit), and a significant increase in percentage of patients with HbA1c less than 7.5%.19
- Transition coordinators. A second more economical approach rather than having a full-fledged transition clinic is to have a separate transition coordinator. The first use of transitional care coordinators was documented from Australia. The coordinators helped to maintain attendance at the dedicated young adult clinic.20 A similar Maestro project in Canada used a systems navigator or “maestro” to help access adult medical care as stand-alone in routine pediatric to adult transition patients. Additionally, the intervention consisted of a website, a regular newsletter, group meetings, and access to especially devised young adult educational events. The program was successful in reducing loss to follow-up and helping older transition patients reconnect with medical care.21
- Young adult support group. Everyone needs a friend in their life, and it is more convenient to communicate with the one who is passing through the same condition as you are. So, forming a young adult group where all these young adults can discuss their issues or even come up with new solutions is yet another way to ease out the transition period. A recent publication has highlighted the utility of support groups for young adults with type 1 diabetes during the transition period. In this study, the participants attended monthly support groups sessions for 5 months. Eighty percent of the participants attended at least three sessions and two-thirds of patients had significant improvements in HbA1c at the end of the program.22
Q4. What is the Ludhiana Model of Transition Care?
At Christian Medical College and Hospital, Ludhiana we use a model that utilizes both a transitional care coordinator and a young adult support group. Children are encouraged to enroll into transition between the ages of 15-16 years and continue to be in the transition group till they are comfortable with our checklist of care/education goals. The transitional coordinator volunteers her time in addition to her primary job as a research associate and helps keep the costs of the care model low. The support group primarily communicates with each other on a WhatsApp group which is moderated by the transitional coordinator. Enrollment into the group is after an informed consent. All transitioning adolescents and young adults have access to a psychologist, but payments must be made if her services are utilized.
Q5. What Are the Primary Principles of Transition?
Regardless of which model is chosen for transition there are some overarching principles that need to be considered when planning out a transition care model. The five principles are summarized in Figure 5. The five Cs of transition are mentioned below:
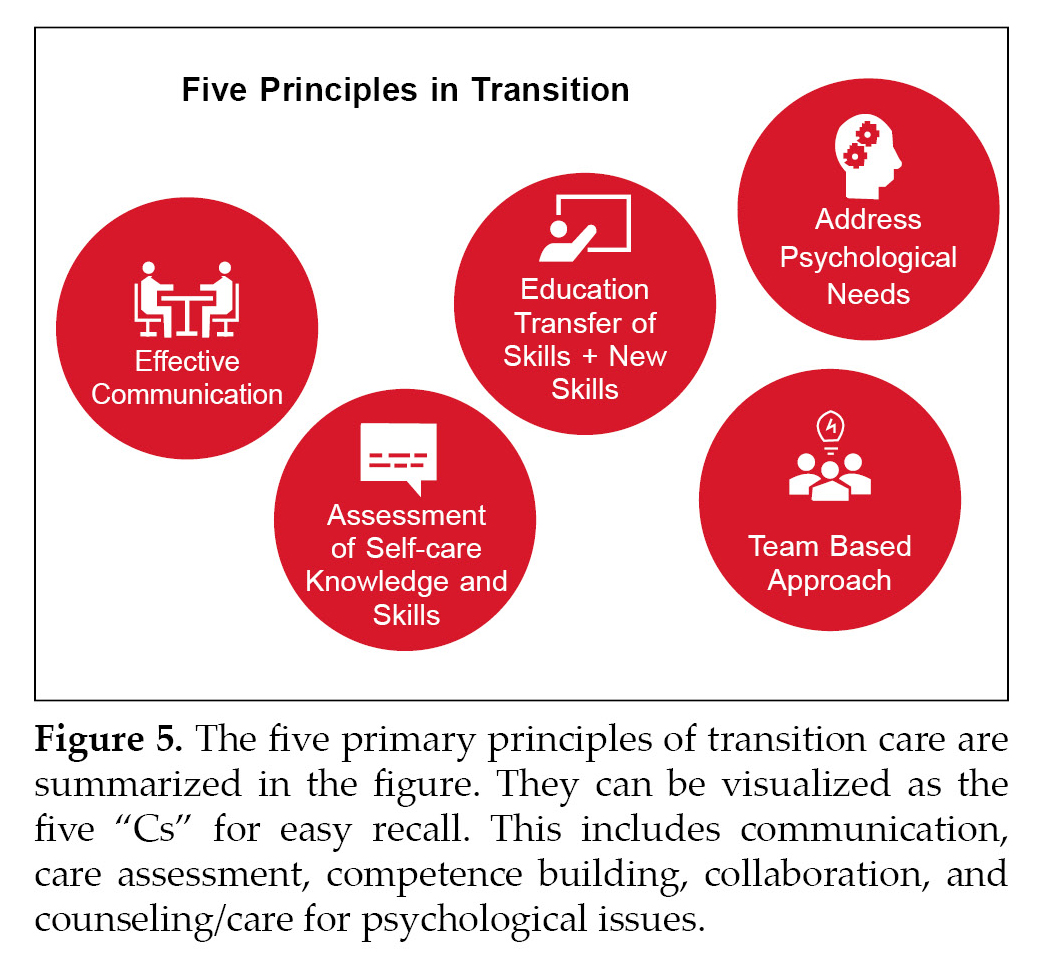
- You need to communicate with the child. To be a favorable communicator you need to adapt the model of active listening where you understand and respond without invalidating the child’s point of view. Ask them about their thoughts on the disease and make them realize the importance of managing it.
- Care (self-knowledge) assessment. This includes a thorough assessment of the child’s knowledge about diabetes and skills required to manage diabetes on a day-to-day basis. It is usually that the family is accountable for the child’s health care prior to adolescence. You can assess their skills through tools like questionnaires in which you can ask about their knowledge about insulin, insulin self-administration, insulin dose adjustments, insulin storage and disposal of sharps. Additionally, skills at self-monitoring, diabetes management if they get sick etc. should be assessed and skills that very likely are available in the family need to be now transferred to the child.
- Competence building. Once self-care knowledge is assessed a plan should be made to transfer this knowledge and skills from the family/health care provider to the child. This may include skills like insulin administration, self-monitoring of glucose and dose adjustments to more complicated skills like making doctor’s appointments, getting medications in time, and having emergency contacts. New skills that need to be provided during transition include safe driving with diabetes, handling stress at work/ schools/examinations, handling peer pressure, safe drinking, and contraceptive advice.
- Cooperation and collaboration. The fourth most important principle of transition is realizing that successful transition needs teamwork of health care professionals, family members and friends. Health care teams could include physicians, diabetes specialist nurses, dieticians, psychologists, podiatrists, and transition coordinators.
- Counseling and caring for psychological issues. As previously mentioned the period of transition is associated with a variety of psychological issues. Many of these require specialized care and appropriate therapy. Transition teams should be able to make this available to children who require this.
Transition period is a vulnerable time for emerging young adults with chronic medical conditions. As adolescents start moving to a different place to gear up for their independent earning, they lose contact with their health care providers which leads to gaps in medical care. There is a large overlap of psychosocial issues so a team-based approach of primary care and psychology would be beneficial. Transition checklists in the clinics can help to address the problems young adults are facing and can ease up the transition process. Awareness and early initiation with a well-structured process for transition is essential.
References
- Jordan A, McDonagh JE. Transition: getting it right for young people. Clin Med (Lond). 2006;6(5):497-500.
- Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000; 55(5):469-80.
- Rosenbloom AL, Wheeler L, Bianchi R, Chin FT, Tiwary CM, Grgic A. Age-adjusted analysis of insulin responses during normal and abnormal glucose tolerance tests in children and adolescents. Diabetes. 1975;24(9):820-8.
- Hannon TS, Janosky J, Arslanian SA. Longitudinal study of physiologic insulin resistance and metabolic changes of puberty. Pediatr Res. 2006;60(6):759-63.
- Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, et al. Assessment of diabetes-related distress. Diabetes Care. 1995;18(6):754-60.
- Reynolds KA, Helgeson VS. Children with diabetes compared to peers: depressed? Distressed? A meta-analytic review. Ann Behav Med. 2011;42(1):29-41.
- Lawrence JM, Standiford DA, Loots B, Klingensmith GJ, Williams DE, Ruggiero A, et al. SEARCH for Diabetes in Youth Study. Prevalence and correlates of depressed mood among youth with diabetes: the SEARCH for Diabetes in Youth study. Pediatrics. 2006;117(4):1348-58.
- Jones JM, Lawson ML, Daneman D, Olmsted MP, Rodin G. Eating disorders in adolescent females with and without type 1 diabetes: cross sectional study. BMJ. 2000;320(7249):1563-6.
- ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 6. Glycemic targets: Standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S97-S110.
- Petitti DB, Klingensmith GJ, Bell RA, Andrews JS, Dabelea D, Imperatore G, et al. SEARCH for Diabetes in Youth Study Group. Glycemic control in youth with diabetes: the SEARCH for diabetes in Youth Study. J Pediatr. 2009;155(5):668-72. e1-3.
- Hoerger TJ, Segel JE, Gregg EW, Saaddine JB. Is glycemic control improving in U.S. adults? Diabetes Care. 2008;31(1):81-6.
- Busse FP, Hiermann P, Galler A, Stumvoll M, Wiessner T, Kiess W, et al. Evaluation of patients’ opinion and metabolic control after transfer of young adults with type 1 diabetes from a pediatric diabetes clinic to adult care. Horm Res. 2007;67(3):132-8.
- Rewers A, Chase HP, Mackenzie T, Walravens P, Roback M, Rewers M, et al. Predictors of acute complications in children with type 1 diabetes. JAMA. 2002;287(19):2511-8.
- Nakhla M, Daneman D, To T, Paradis G, Guttmann A. Transition to adult care for youths with diabetes mellitus: findings from a Universal Health Care System. Pediatrics. 2009;124(6):e1134-41.
- McGill HC Jr, McMahan CA, Zieske AW, Sloop GD, Walcott JV, Troxclair DA, et al. The Pathobiological Determinants of Atherosclerosis in Youth Research Group. Associations of coronary heart disease risk factors with the intermediate lesion of atherosclerosis in youth. Arterioscler Thromb Vasc Biol. 2000;20(8):1998-2004.
- Laing SP, Swerdlow AJ, Slater SD, Botha JL, Burden AC, Waugh NR, et al. The British Diabetic Association Cohort Study, I: all-cause mortality in patients with insulin-treated diabetes mellitus. Diabet Med. 1999;16(6):459-65.
- Lane JT, Ferguson A, Hall J, McElligott M, Miller M, Lane PH, et al. Glycemic control over 3 years in a young adult clinic for patients with type 1 diabetes. Diabetes Res Clin Pract. 2007;78(3):385-91.
- Holmes-Walker DJ, Llewellyn AC, Farrell K. A transition care programme which improves diabetes control and reduces hospital admission rates in young adults with type 1 diabetes aged 15-25 years. Diabet Med. 2007;24(7):764-9.
- Logan J, Peralta E, Brown K, Moffett M, Advani A, Leech N. Smoothing the transition from paediatric to adult services in type 1 diabetes. J Diabetes Nurs. 2008;12(9):328-38
- Van Walleghem N, Macdonald CA, Dean HJ. Evaluation of a systems navigator model for transition from pediatric to adult care for young adults with type 1 diabetes. Diabetes Care. 2008;31(8):1529-30.
- Cadario F, Prodam F, Bellone S, Binotti M, Trada M, Allochis G, et al. Transition process of patients with type 1 diabetes (T1DM) from pediatric to the adult health care service: a hospital-based approach. Clin Endocrinol (Oxf). 2009;71(3):346-50.
- Markowitz JT, Laffel LMB. Transitions in care: support group for young adults with type 1 diabetes. Diabet Med. 2012;29(4):522-5.
|