
Introduction
Diabetes care is a complex affair. The vast diversity of the causative factors, clinical features and concerns that a person presents with, along with the equally diverse complications, comorbidities and concomitant medications that may coexist with diabetes, make management challenging. One way of meeting this is to classify diabetes in a manner which helps in therapeutic planning.
Rubrics of Classification
Various rubrics have been proposed by expert clinicians and researchers to assist in this endeavor. The simplest, perhaps, is the metabolic fulcrum, which divides persons with diabetes into those who are catabolic ‘eubolic’, and those who are ‘maladaptively anabolic.1 This is concordant with the tridoshic concept of Ayurveda, which lists vata, pitta and kapha as the three doshas.2
Catabolism can be viewed as an equivalent of vata, embolism as pitta, while maladaptive anabolism can be viewed as kapha. While the metabolic fulcrum is based upon phenotype and physiology, it is backed by biochemistry, and promotes person-centred choice of pharmacotherapy as well.
Recently, researchers have suggested five clusters of diabetes: severe autoimmune diabetes, severe insulin deficient diabetes, severe insulin resistant diabetes, mild obesity related diabetes and mild age-related diabetes.3
Insulin resistant obese diabetes is also reported from India, as is combined insulin resistant and deficient diabetes.4
Advantages of Phenotyping
These phenotypes assist in not only classifying, but also managing diabetes. Identifying the specific phenotype allows the clinician to anticipate the natural trajectory of the syndrome, counsel the patient and advise appropriate screening, monitoring and therapeutic interventions. There is much more to diabetes than mere biochemistry, however. The individual’s attitude towards the health care system influences the natural history of diabetes as much as biomedical factors do. Health care seeking, and health care accepting behaviors contribute to the success, or otherwise, of any diabetes care strategy. Accepting the diagnosis of diabetes, and prescribed treatments, are the rate-limiting step of the diabetes care pathway. Emotional and social factors play an important role in this process.5
Sapiotyping
We propose the term ‘Sapiotype’, based on the Latin root ‘sapiens’ (wise) to describe the various attitudes that persons with diabetes may have towards their disease, their doctor or health care providers, a specific diagnostic procedure, drug or delivery device, and the health care system at large.
Understanding the sapiotype assists the diabetes care professional in understanding the mental makeup of the individual being treated, in crafting effective communication and counseling strategies and in planning person-centric therapeutic interventions. We list these sapiotypes in Table 1, providing an alliterative rubric that can be used in the clinic.
Just as we compare the metabolic triad with the Ayurvedic tridoshic model, we attempt to link sapiotypes to the three mental and emotional phenotypes of Indian philosophy: Rajsik, sativik and tamsik.6 While rajsik conveys an action-oriented, androgenic and adrenergic mindset; tamsik describes the opposite-complacence, casualness and callousness. Sativik is a balanced state, characterized by equanimity and equipoise.
Sapiotypic Spectrum
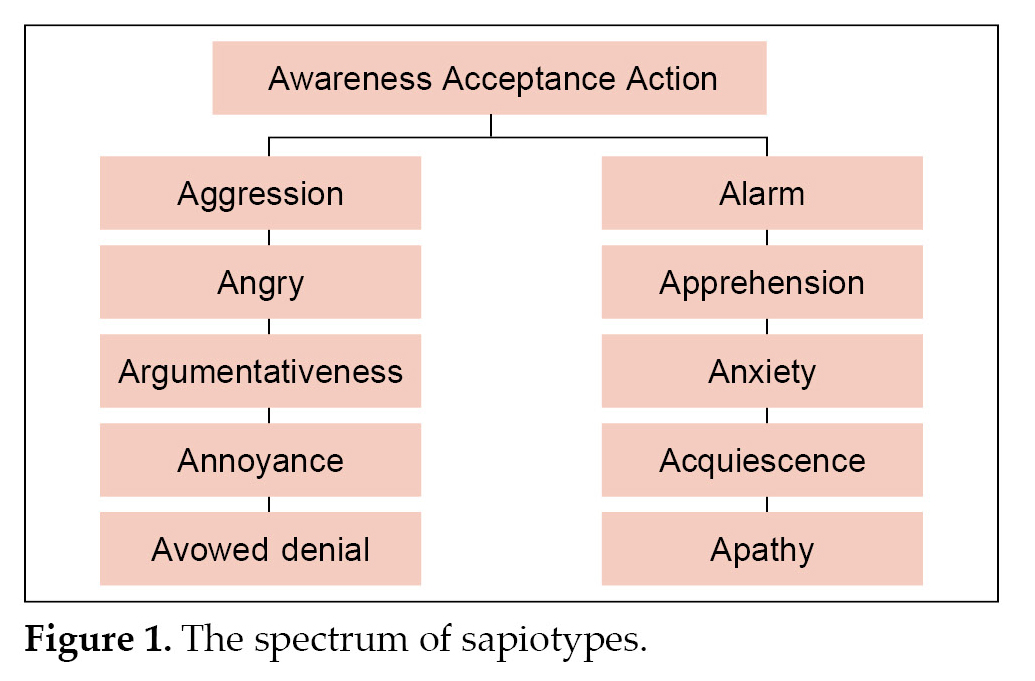
The sapiotype may be viewed as a spectrum of emotions (Figure 1), ranging from extreme denial and anger on one hand, to extreme apathy and fatalism on the other. The zone in the middle-acceptance, affirmative assertion and action, in anticipation of better health, is the ideal state of mind for health care.
Sapiotypic Fluidity
No single emotion can exist in isolation and neither can it be sustained lifelong. The same person may exhibit varied emotions to different targets (e.g., members of the health care team; specific investigations and medications) at various times during the journey of diabetes. These variations should be accepted as a part of emotional fluidity. However, there will always be a single emotion that will predominate at the start of any clinical encounter. This is the sapiotype of the individual at that point of time.
The sapiotype is malleable, and can be molded and modified to optimize therapeutic outcomes. Knowing where one starts from can help the astute clinician guide the patient, using a process of informed and shared decision making, towards optimal health. This is the process of responsible person centered care.
The Way Forward
We suggest the use of sapiotypes in clinical practice, as well as in research, to create person-centered therapeutic counseling and education interventions, The sapiotypic model also allows for institution of appropriate pharmacological therapy, as it includes
|
Table 1. Sapiotypes Encountered in Health Care
|
|
Sapiotype
|
Equivalent in Indian philosophy
|
|
Avowed denial
|
Tamsik
|
|
Annoyed/angry
Aggressive/argumentative
|
Rajsik
|
|
Accepting/aware/
Action oriented
|
Sativik
|
|
Anxious/afraid (diabetes distress, insulin distress)/alarmed
|
Rajsik
|
|
Apathic/acquiescent (fatalistic)
|
Tamsik
|
the clinical constructs of diabetes distress and insulin distress. The first step, however, would be to create and validate screening and diagnostic tools to help identify sapiotypes. Once this is done, sapiotypic characterization will become part of evidence-based medicine.
References
- Kalra S, Gupta Y. Choosing injectable therapy: the metabolic fulcrum. J Pak Med Assoc. 2016;66(7):908-9.
- Pal M. The tridosha theory. Anc Sci Life. 1991;10(3):144-55.
- Ahlqvist E, Storm P, Käräjämäki A, Martinell M, Dorkhan M, Carlsson A, et al. Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysis of six variables. Lancet Diabetes Endocrinol. 2018;6(5):361-9.
- Anjana RM, Pradeepa R, Unnikrishnan R, Tiwaskar M, Aravind SR, Saboo B, et al. New and unique clusters of type 2 diabetes identified in Indians. J Assoc Physicians India. 2021;69(2):58-61.
- Kalra S, Sridhar GR, Balhara YP, Sahay RK, Bantwal G, Baruah MP, et al. National recommendations: Psychosocial management of diabetes in India. Indian J Endocrinol Metab. 2013;17(3):376-95.
- Satpathy B. Pancha Kosha theory of personality. Int J Indian Psych. 2018;6(2):33-9.