Abstract
Background: Stroke is a leading cause of mortality and disability globally. Diabetes mellitus increases the risk of stroke. It has been observed that the risk of stroke is usually higher among the young diabetic patients. Prediabetic patients are also at risk of stroke as the presence of glucose in blood results in vascular endothelial dysfunction, increased early-age arterial stiffness, systemic inflammation and thickening of the capillary basal membrane. In this prospective observational study we aimed to determine the association between triglyceride glucose (TyG) index in type-2 diabetes mellitus patients and acute ischemic stroke. Methods: A total of 75 patients with acute ischemic stroke and history of diabetes mellitus during the period of study were included in the study. Results: The mean age of the patients was 58.74 ± 11.37 years and the majority of the patients were males (57%) with 43% females. The average National Institutes of Health Stroke Scale (NIHSS) score of study participants was 5. The mean fasting plasma glucose (FPG) value was as 6.13 ± 2.03 (mmol/L), mean total cholesterol (TC) was 5.76 ± 1.4 (mmol/L), mean triglyceride (TG) 1.98 ± 0.93 was (mmol/L) and mean TyG index was 8.76 ± 0.28. Conclusion: The present study concluded that the TyG index is an important risk factor of ischemic stroke as it was observed that the patients with higher TyG index has higher incidence of ischemic stroke.
Keywords: Diabetes, glucose level, triglycerides, ischemia and stroke.
Introduction
Diabetes is known as silent killer, which can start from early stages of life and can be asymptomatic.
It is a chronic noncommunicable1 disease characterized by a state of chronic hyperglycemia, resulting from diverse etiologies, the environment and genetic, acting jointly. The underlying cause of diabetes is the defective production or action of insulin, a hormone that controls glucose, fat and amino acid metabolism with variable clinical manifestations and progression.
Diabetes mellitus increases the risk of stroke. It was observed that the risk of stroke is usually higher among the young diabetic patients. According to the Greater Cincinnati/Northern Kentucky stroke study, diabetes mellitus increases the risk and incidence of ischemic stroke among all age groups, but this risk is most striking before the age of 55 years in African Americans and before the age of 65 years in whites.2
Prediabetic patients are also at risk of stroke as the presence of glucose in blood results in vascular endothelial dysfunction, increased early-age arterial stiffness, systemic inflammation and thickening of the capillary basal membrane.3
Stroke is a leading cause of mortality and disability globally.4 There are multiple risk factors or associated conditions resulting in stroke. Literature suggests that insulin resistance enhances progression of stroke and is also associated with poor prognosis.
Triglyceride glucose (TyG) index is used to measure insulin resistance and is derived from fasting blood glucose and triglycerides.5
Several studies have concluded that high triglyceride index is an important predictor of mortality and outcome of acute ischemic stroke.6
Thus, the present study was undertaken to elucidate the association between TyG index acute ischemic stroke in patients with type 2 diabetes.
Material and Methods
This prospective observational study was done in the Department of Medicine in Acharya Shri Chander College of Medical Sciences and Hospital, Jammu, from January 2022 to February 2023 after obtaining approval from the Institutional Ethics Committee.
A total of 75 patients with acute ischemic stroke and history of diabetes mellitus during the period of study were included in the study.
Detailed clinical examination followed by routine laboratory and radiographic investigations were carried out in all cases. A detailed history including demographic variables, medication history, past history of illness, etc. was collected.
Blood samples were collected for TyG index and fasting blood sugar (FBS).
Data was organized, tabulated, analyzed and interpreted in both descriptive and inferential statistics i.e. frequency and percentage distribution, mean by using statistical package for social sciences (SPSS) software version 21. Categorical variables were expressed as number and percentage.
Observations and results
In the present study, 75 cases with acute ischemic stroke and history of diabetes mellitus were evaluated.
The mean age of the patients was 58.74 ± 11.37 years and the majority of the patients were males (57%) followed by 43% females. The average NIHSS score of study participants was 5.
The observed mean systolic blood pressure (SBP) was 145 ± 26.3 mmHg and mean diastolic blood pressure (DBP) was 90.2 ± 18.6 mmHg as depicted in Table 1.
Fifty-two percent of the patients were smokers as shown in Figure 1.
In our study, 69.33% subjects were on antidiabetic drugs, followed by antihypertensives (61.33%), lipid lowering drugs (50.66%), anticoagulants (16%) and antiplatelets (14.66%) as depicted in Table 2.
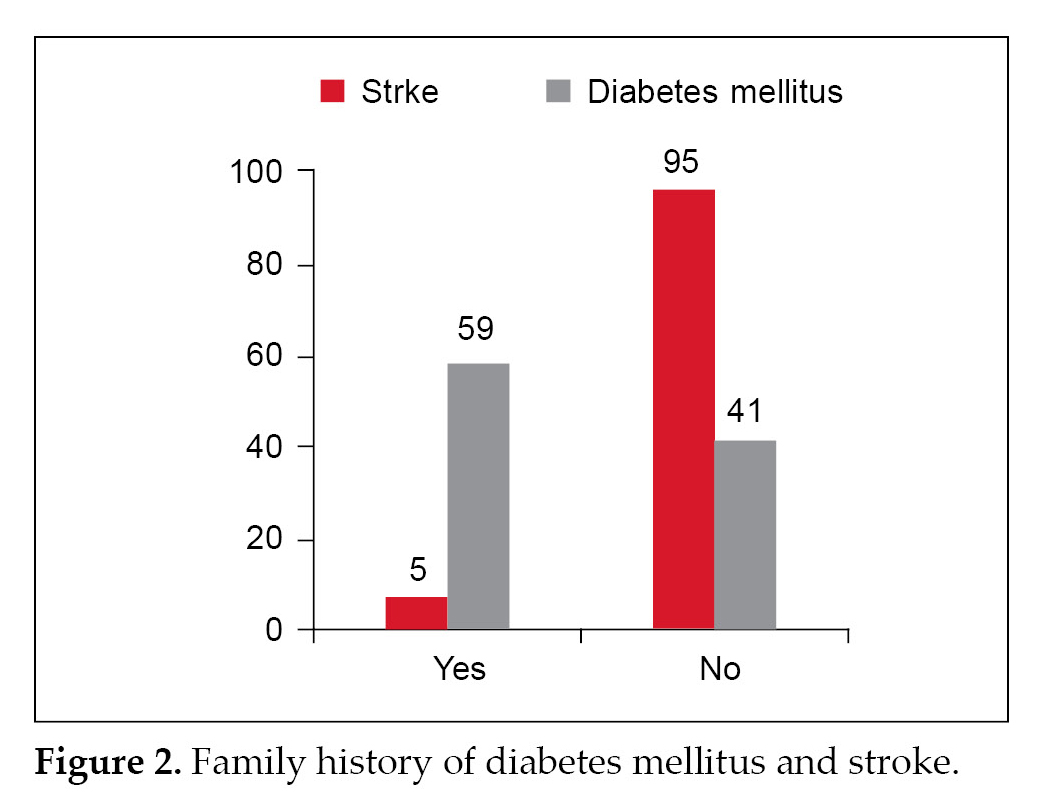
Figure 2 represents that 59% patients had family history of diabetes mellitus and 5% patients had family history of stroke.
The mean fasting plasma glucose (FPG) value was 6.13 ± 2.03 (mmol/L), mean total cholesterol (TC) was
|
Table 1. Blood Pressure
|
|
|
Blood pressure
|
Mean ± SD
|
|
SBP (mmHg)
|
145 ± 26.3
|
|
DBP (mmHg)
|
90.2 ± 18.6
|
|
Table 2. Drug History
|
|
|
Drug
|
No. of cases
|
Percentage
|
|
Antidiabetic
|
52
|
69.33
|
|
Anticoagulants
|
12
|
16
|
|
Antihypertensive
|
46
|
61.33
|
|
Lipid lowering drugs
|
38
|
50.66
|
|
Antiplatelets
|
11
|
14.66
|
|
Table 3. Laboratory Findings
|
|
Parameters
|
Mean ± SD
|
|
FPG (mmol/L)
|
6.13 ± 2.03
|
|
TC (mmol/L)
|
5.76 ± 1.4
|
|
TG(mmol/L)
|
1.98 ± 0.93
|
|
TyG index
|
8.76 ± 0.28
|
|
Table 4. TyG Index vs. Stroke
|
|
TyG index
|
Incidence of stroke N (%)
|
P value
|
|
Q1 (4.31-5.48)
|
10 (13.33)
|
0.27
|
|
Q2 (5.48-5.81)
|
15 (20)
|
0.21
|
|
Q3 (5.81-6.22)
|
21 (28)
|
0.04
|
|
Q4 (6.22-8.17)
|
29 (38.66)
|
0.03
|
5.76 ± 1.4 (mmol/L), mean triglyceride (TG) 1.98 ± 0.93 was (mmol/L) and mean TyG index was 8.76 ± 0.28 as depicted in Table 3.
Table 4 shows that the patients with higher TyG index showed a higher incidence of stroke (p = 0.03).
Discussion
In our study the mean age of the patients was 58.74 ± 11.37 years and the majority of the patients were males (57%) followed by 43% females. The average NIHSS score of study participants was 5. It was reported that the most of the patients were smoker. These observations correlate with the study by Liu, et al (2022)7 who found that the mean age of the study participants was 65.0 (57.0-73.0) years, most of the patients were males (59.2%) and the median NIHSS score was 4.0 (2.0-7.0). Toh, et al; (2022)8 found that the most of the patients were males (61.5%), the median age of the patients was 65.00 (55.00, 76.00) years and the median NIHSS score was 6.0 (2.0, 15.0). Zhou, et al (2020) found that 44.4% subjects were smoker.9
The observed mean SBP was 145 ± 26.3 mmHg and mean DBP was 90.2 ± 18.6 mmHg. 59% patients had family history of diabetes mellitus and 5% patients had family history of stroke. These findings are consistent with the study by Zhou, et al (2020)9 who reported that the mean SBP and DBP was 149.2 ± 23.0 mmHg and 87.44 ± 13.4 mmHg. Kourtidou, et al (2022) also observed that the mean SBP and DBP was 151 ± 27 mmHg and 81 ± 15 mmHg.10
Present study showed that 69.33% subjects were on antidiabetic drugs, followed by antihypertensive (61.33%), lipid-lowering drugs (50.66%), anticoagulants (16%) and antiplatelets (14.66%).
These findings are similar to the study conducted by Zhou, et al (2020)9 who found that 19.6% subjects were on antiplatelet drug, 1% were on anticoagulants 44.9% were on antihypertensive drugs, 6.8% were on lipid-lowering drugs and 16.0% were on hypoglycemic agents.
The mean FPG value in the present study was 6.13 ± 2.03 (mmol/L), mean TC was 5.76 ± 1.4 (mmol/L), mean TG 1.98 ± 0.93 was (mmol/L) and mean TyG index was 8.76 ± 0.28. These results are in accordance with the study conducted by Guo, et al (2021)11 who found that the mean fasting glucose value was 4.9, 5.1, 5.4 and 7.1 (mmol/L) among 4 groups, mean TC was 1.0, 1.2. 1.4 and 1.6 (mmol/L) among 4 groups, and mean TG was 2.5, 3.3, 4.0 and 4.6 (mmol/L) among 4 groups. Zhou, et al (2020)9 found that the mean TG was 119.5 (mg/dL) and mean FBS was 114.1 ± 46.9 (mg/dL).
The present study showed that the patients with higher TyG index showed a higher incidence of stroke (p = 0.03). These findings correlate with the studies conducted by Liu, et al (2022)7, Toh, et al (2022)8, Hu, et al (2022)12 and Zhou, et al (2020)9 who reported significant association between TyG index in type 2 diabetes mellitus patients and acute ischemic stroke.
Conclusion
The present prospective study found that there was significant association between TyG index in type 2 diabetes mellitus patients and acute ischemic stroke. Thus, it is concluded that the TyG index is an important risk factor of ischemic stroke.
References
- World Health Organization (WHO). Global status report on noncommunicable diseases 2010. World Health Organization. Available from: https://apps.who.int/iris/handle/10665/44579.
- Khoury JC, Kleindorfer D, Alwell K, Moomaw CJ, Woo D, Adeoye O, et al. Diabetes mellitus: a risk factor for ischemic stroke in a large biracial population. Stroke. 2013;44(6):1500-4.
- Chen R, Ovbiagele B, Feng W. Diabetes and stroke: epidemiology, pathophysiology, pharmaceuticals and outcomes. Am J Med Sci. 2016;351(4):380-6.
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28-e292.
- Sánchez-García A, Rodríguez-Gutiérrez R, Mancillas-Adame L, González-Nava V, Díaz González-Colmenero A, Solis RC, et al. Diagnostic accuracy of the triglyceride and glucose index for insulin resistance: A systematic review. Int J Endocrinol. 2020;2020:4678526.
- Ma X, Han Y, Jiang L, Li M. Triglyceride-glucose index and the prognosis of patients with acute ischemic stroke: a meta-analysis. Horm Metab Res. 2022;54(6):361-70.
- Liu D, Yang K, Gu H, Li Z, Wang Y, Wang Y, et al. Predictive effect of triglyceride-glucose index on clinical events in patients with acute ischemic stroke and type 2 diabetes mellitus. Cardiovasc Diabetol. 2022;21(1):280.
- Toh EMS, Lim AYL, Ming C, Yeo LLL, Sia CH, Tan BWQ, et al. Association of triglyceride-glucose index with clinical outcomes in patients with acute ischemic stroke receiving intravenous thrombolysis. Sci Rep. 2022;12(1):1596.
- Zhou Y, Pan Y, Yan H, Wang Y, Li Z, Zhao X, et al. Triglyceride glucose index and prognosis of patients with ischemic stroke. Front Neurol. 2020;11:456.
- Kourtidou C, Ztriva E, Kostourou DT, Polychronopoulos G, Satsoglou S, Chatzopoulos G, et al. The predictive role of the triglyceride/glucose index in patients with hypercholesterolemia and acute ischemic stroke. Rev Cardiovasc Med. 2022;23(12):399.
- GuoY, Zhao J, Zhang Y, Wu L, Yu Z, He D, et al. Triglyceride glucose index influences platelet reactivity in acute ischemic stroke patients. BMC Neurol. 2021;21(1):409.
- Hu L, Bao H, Huang X, Zhou W, Wang T, Zhu L, et al. Relationship between the triglyceride glucose index and the risk of first stroke in elderly hypertensive patients. Int J Gen Med. 2022;15:1271-79.