Abstract
Co-occurrence of multiple sclerosis with type 2 diabetes mellitus with lepromatous leprosy is rare. We hereby report a case of multiple sclerosis with type 2 diabetes mellitus with lepromatous leprosy in a middle-aged female. She was clinically diagnosed as having multiple sclerosis with type 2 diabetes mellitus and presented with fever, ENL and neuritis. Her MRI reports were normal but she had a positive slit-skin smear and skin biopsy as lepromatous leprosy. Proceeding with this diagnosis, she was treated with baclofen for spastic bladder, antibiotics for urinary tract infection, oral hypoglycemic agents and oral steroids with multibacillary treatment for leprosy with type 2 reactions. She responded well and currently is being followed-up.
Keywords: Multiple sclerosis, leprosy, diabetes mellitus, demyelinating neuropathy
Introduction
Multiple sclerosis is a disorder with heterogeneous clinical and pathologic features reflecting various pathways to tissue injury.1 Inflammation, demyelination and axonal degeneration are the key pathologic mechanisms, which lead to clinical manifestations.2,3 However, the cause of multiple sclerosis remains unknown.4,5 The most widely accepted theory suggests that it begins as an inflammatory immune-mediated disorder characterized by autoreactive lymphocytes.1,6 Later, the disease is dominated by microglial activation and chronic neurodegeneration.2
Leprosy (Hansen’s disease) is an infectious disease caused by Mycobacterium leprae that involves the skin and peripheral nerves. Early diagnosis and a full course of treatment are critical for preventing lifelong neuropathy and disability.7 Although the infection is highly responsive to treatment, leprosy became an important global health concern due to deformities and disabilities of the eyes, hands and feet secondary to neuropathy which are often irreversible and require lifelong care and rehabilitation. Therefore, early diagnosis and management are necessary to minimize the likelihood of these disabilities.8
Type 2 diabetes mellitus is characterized by hyperglycemia, insulin resistance and relative impairment in insulin secretion. It is a common disorder with a prevalence that rises markedly with increasing degrees of obesity.9
The prevalence of type 2 diabetes has risen alarmingly in the past decade,10 in large part linked to the trends in obesity and sedentary lifestyle.11
Case Report
A 55-year-old female was brought by her relatives to the skin department. She had flexor spasms, difficulty in walking, spastic bladder with an indwelling catheter since last 4 years and was diagnosed to have multiple sclerosis. She had multiple admissions for fever and urinary tract infection and was on oral hypoglycemic
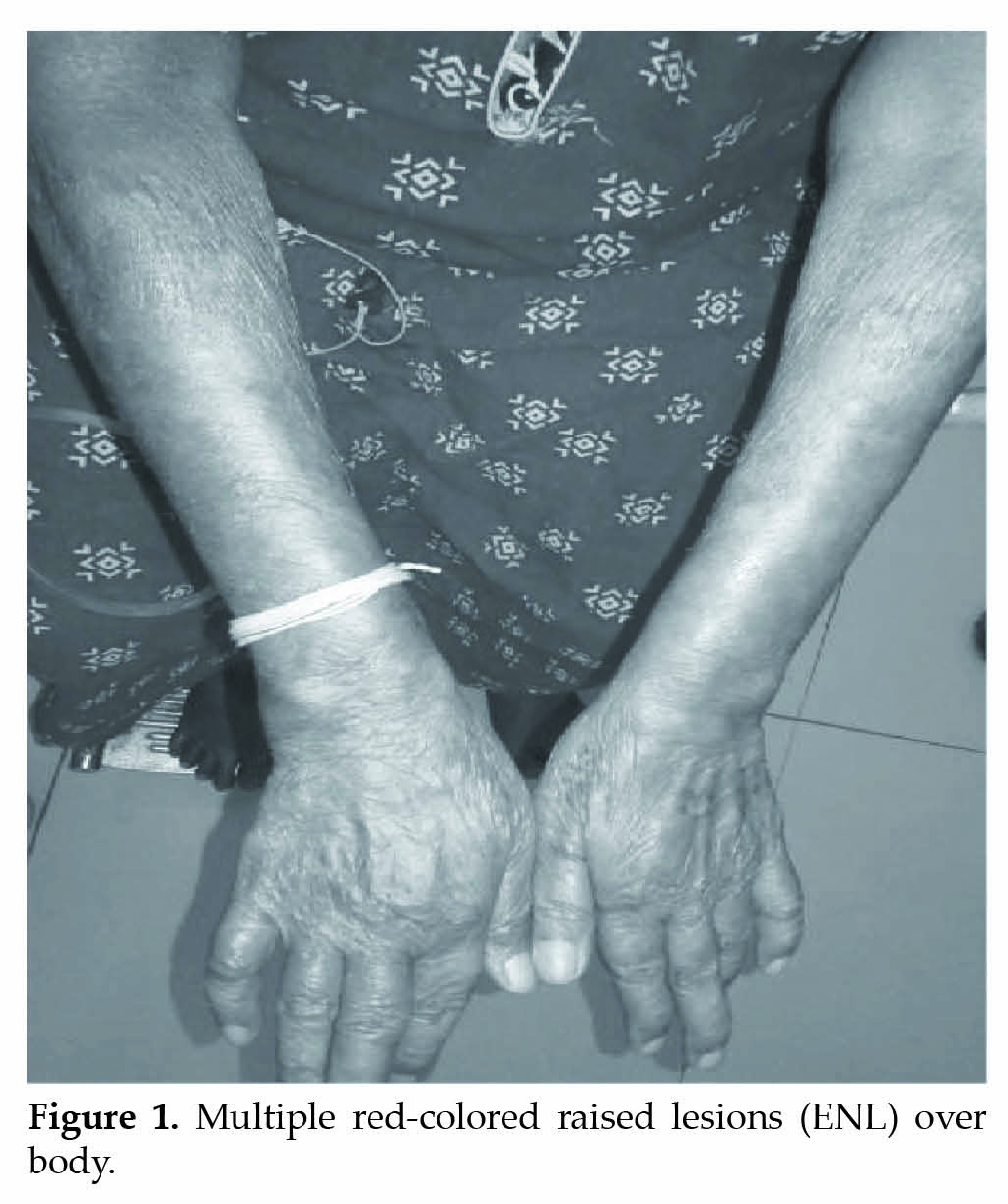

agents on regular basis. She presented with fever, multiple red-colored raised lesions (Erythema nodosum leprosum or ENL) all over the body (Fig. 1), with weakness, tingling and numbness over both upper and lower limbs. ENL were also present over her face
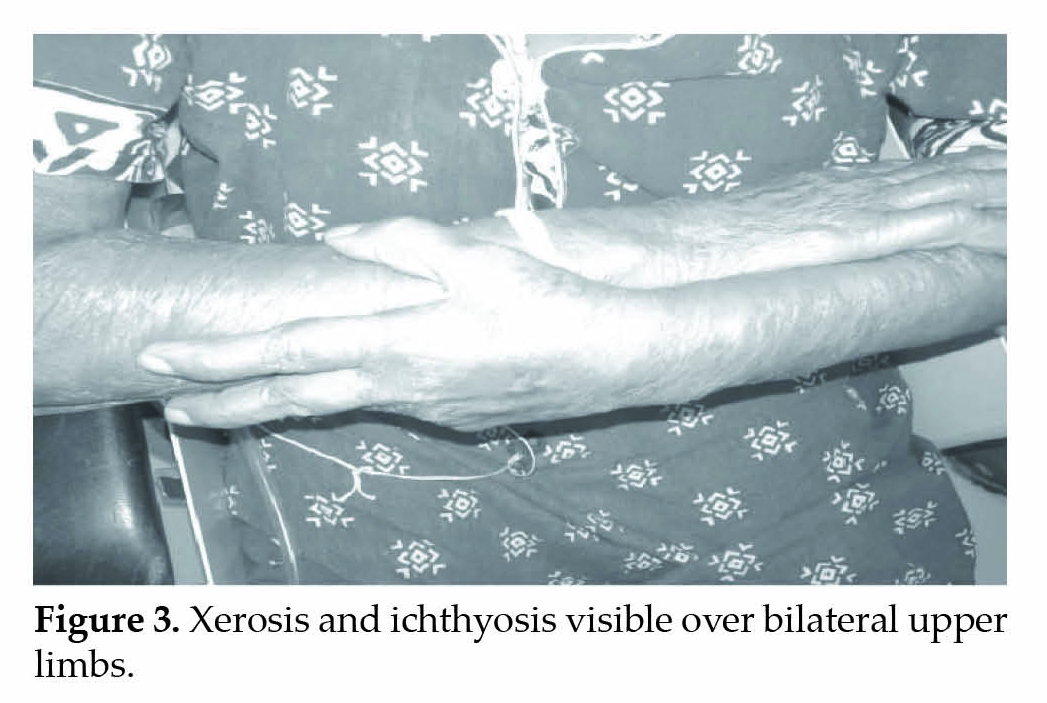
adjacent to the angle of mouth (Fig. 2). Xerosis and ichthyosis characteristic of leprosy was visible over bilateral upper limbs (Fig. 3). There was no history of photosensitivity or any drug intake or application of any local irritant prior to the initial lesion.
Her detailed central nervous system evaluation revealed upper motor neuron type of paraparesis, sensorimotor with proximal as well as distal muscle involvement with urge incontinence suggestive of spastic type of neurogenic bladder. Her mental functions were intact with no cranial nerve involvement. Cardiovascular system, respiratory system and per abdominal evaluation was within normal limits.
Her routine blood biochemistry was normal except for low hemoglobin levels (5.9%), raised white blood cell (WBC) counts (15,800) and raised random blood sugar (RBS) levels (157 mg/dL). Urine analysis revealed urinary tract infection for which she was treated with antibiotics. Bladder care was given. She was treated with baclofen. Skin examination revealed positive slit-skin smear for acid-fast bacilli with bacteriological index of 3.5 and skin biopsy consistent with lepromatous leprosy. She was put on oral steroids for type 2 lepra reaction and multibacillary anti-leprosy treatment for leprosy. Appropriate oral hypoglycemic agents were continued as she was reluctant with insulin administration. Brain imaging was normal. She responded well and her flexor spasms decreased. A psychiatric consultation was sought for her depression due to chronic illness and was started on antidepressants.
Discussion
Dominant or recessive genetic mutations give rise to a number of inherited neuropathies. The basic pathology happens to be in the Schwann cells, the myelinating unit of the neuron leading to defective myelination, alteration of the axonal cytoskeleton and disruption of the axonal transport.12 Genes involved in the axonal transport are the chief site of mutation in the majority of inherited neuropathies leading to the atrophy of the axons and directly correlate with the clinical features in the inherited neuropathies.12 Diabetes mellitus is characterized by a number of sensorimotor and mixed neuropathies. The pathologic hallmark of neuropathies occurring in long-term diabetics involves the advanced glycation end products, persistent oxidative stress, polyol pathway flux and protein kinase C activation, ultimately contributing to microvascular disease and nerve dysfunction.13
Common symptoms of multiple sclerosis include sensory abnormalities including pain, motor symptoms due to involvement of the pyramidal tracts, visual disturbances, ataxia and Lhermitte sign. The pattern of abnormalities can vary from subtle limb weakness or sensory symptoms like Uhthoff phenomenon to more severe sensorimotor noncompressive myelopathies like acute transverse myelitis. Retrobulbar neuritis and optic neuritis have been the common causes of transient visual disturbances in multiple sclerosis. The onset is often polysymptomatic. Neuropathy is an early feature in Hansen’s disease, as earliest diagnostic lesions are characterized by hypoesthesia.14 Though early sensory loss is a common finding in leprosy, in some cases, patients can present with pain, which is often late in the course of the disease.15,16
In the tuberculoid spectrum of the Ridley-Jopling classification, neuropathy occurs in the proximity of the skin lesions, as against neuropathy in lepromatous disease, which is more generalized. Common nerves include the ulnar, median nerves (claw hand), the common peroneal nerve (foot drop), the posterior tibial nerve (claw toes and plantar insensitivity), the facial nerve (lagophthalmos), the radial cutaneous nerve, and the great auricular nerve. Subclinical neuropathy is found more commonly, as against it was previously believed in leprosy. These results may have implications for the design of ErbB2 RTK-based therapies for both leprosy nerve damage and other demyelinating neurodegenerative diseases.17
Here we report this case as to the best of our knowledge, leprosy with multiple sclerosis has not been reported in literature.
Conclusion
Multiple sclerosis, Hansen’s disease and diabetes mellitus are multisystem diseases with distinct etiologies affecting the sensory as well as motor nerve fibers. It is considerably rare to find a demyelinating, infectious and autoimmune disease of the nerves to coexist in the same patient. All these conditions can be managed simultaneously and successfully.
References
- Weiner HL. Multiple sclerosis is an inflammatory T-cell-mediated autoimmune disease. Arch Neurol. 2004;61(10):1613-5.
- Compston A, Coles A. Multiple sclerosis. Lancet. 2008;372(9648):1502-17.
- Dendrou CA, Fugger L, Friese MA. Immunopathology of multiple sclerosis. Nat Rev Immunol. 2015;15(9):545-58.
- Goodin DS. The epidemiology of multiple sclerosis: insights to disease pathogenesis. Handb Clin Neurol. 2014;122:231-66.
- Nylander A, Hafler DA. Multiple sclerosis. J Clin Invest. 2012;122(4):1180-8.
- Roach ES. Is multiple sclerosis an autoimmune disorder? Arch Neurol. 2004;61(10):1615-6.
- Global leprosy situation, 2010. Wkly Epidemiol Rec. 2010;85(35):337-48.
- WHO Global Leprosy Strategy agreed for 2011-2015. Available at: www.searo.who.int/EN/Section980/Section2572/Section2578_14961.htm.
- Harris MI. Impaired glucose tolerance in the U.S. population. Diabetes Care. 1989;12(7):464-74.
- Engelgau MM, Geiss LS, Saaddine JB, Boyle JP, Benjamin SM, Gregg EW, et al. The evolving diabetes burden in the United States. Ann Intern Med. 2004;140(11):945-50.
- Sullivan PW, Morrato EH, Ghushchyan V, Wyatt HR, Hill JO. Obesity, inactivity, and the prevalence of diabetes and diabetes-related cardiovascular comorbidities in the U.S., 2000-2002. Diabetes Care. 2005;28(7):1599-603.
- Suter U, Scherer SS. Disease mechanisms in inherited neuropathies. Nat Rev Neurosci. 2003;4(9):714-26.
- Duby JJ, Campbell RK, Setter SM, White JR, Rasmussen KA. Diabetic neuropathy: an intensive review. Am J Health Syst Pharm. 2004;61(2):160-73; quiz 175-6.
- Scollard DM, Adams LB, Gillis TP, Krahenbuhl JL, Truman RW, Williams DL. The continuing challenges of leprosy. Clin Microbiol Rev. 2006;19(2):338-81.
- Saunderson P, Bizuneh E, Leekassa R. Neuropathic pain in people treated for multibacillary leprosy more than ten years previously. Lepr Rev. 2008;79(3):270-6.
- Lasry-Levy E, Hietaharju A, Pai V, Ganapati R, Rice AS, Haanpää M, et al. Neuropathic pain and psychological morbidity in patients with treated leprosy: a cross-sectional prevalence study in Mumbai. PLoS Negl Trop Dis. 2011;5(3):e981.
- Tapinos N, Ohnishi M, Rambukkana A. ErbB2 receptor tyrosine kinase signaling mediates early demyelination induced by leprosy bacilli. Nat Med. 2006;12(8):961-6.