Abstract
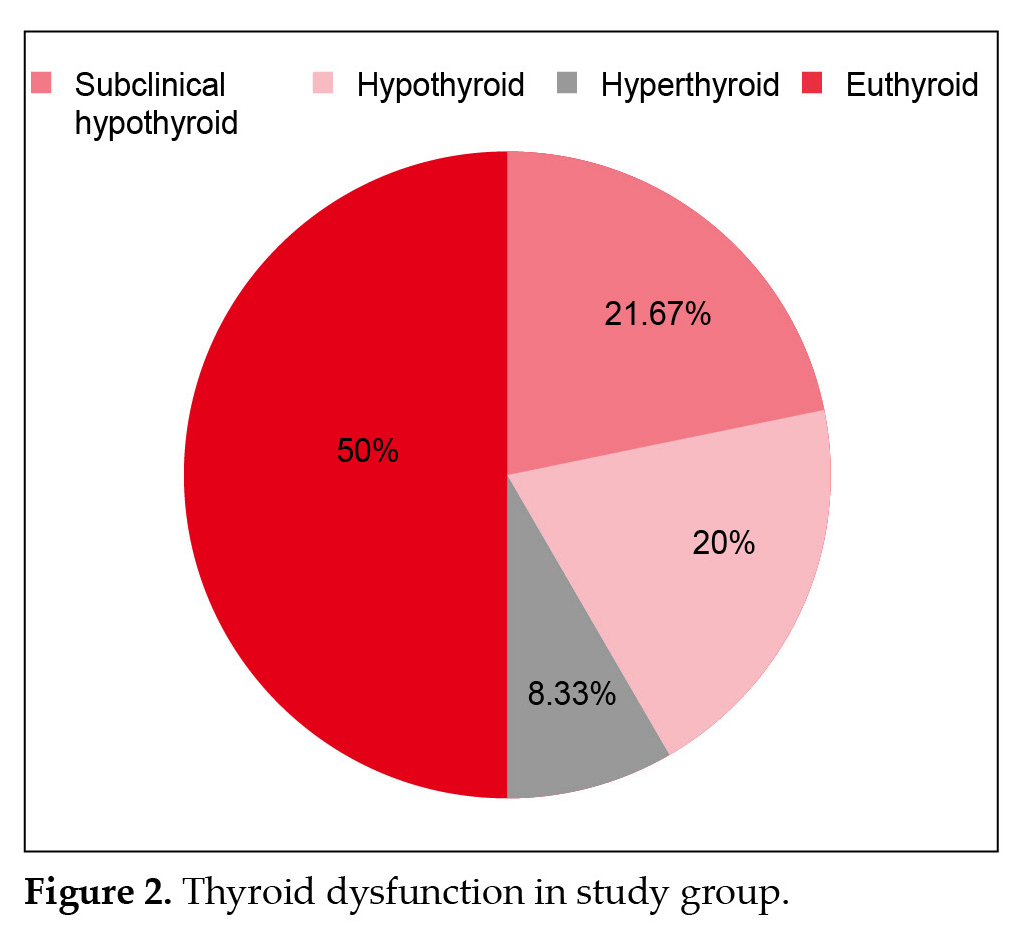
Background: The metabolic syndrome is a constellation of clinical and metabolic abnormalities including abdominal obesity, hypertension, dyslipidemia and impaired fasting glucose or impaired glucose tolerance. Metabolic syndrome and thyroid dysfunction are independent risk factors for cardiovascular disease. Aims and objectives: To study the prevalence, symptomatology of thyroid dysfunction and fine needle aspiration cytology (FNAC) findings of thyroid in the patients having metabolic syndrome. Material and methods: The study was carried out in 60 cases of metabolic syndrome (according to NCEP ATP III criteria) selected from the medicine outdoor clinic (including diabetic clinics, thyroid clinics) and medicine indoor wards in Post Graduate Department of Medicine, SN Medical College and Hospital, Agra. Diagnosis of thyroid dysfunction was made by history, examination and serum FT4 and TSH. Result and observations: Out of 60 patients of metabolic syndrome, 30 patients (50%) were euthyroid, 13 patients (21.66%) had subclinical hypothyroid and 12 patients (20%) had overt hypothyroid. Five patients (8.33%) of metabolic syndrome had hyperthyroidism. Truncal obesity was most prevalent (80.0%) component of metabolic syndrome, followed by hypertriglyceridemia (70%). Diabetes mellitus was equally prevalent in both males as well as females and was present in about 40.0% patients and 53% of patients with metabolic syndrome were hypertensive. Conclusion: This study shows that 50% metabolic syndrome patients had thyroid dysfunction. About 21.66% had subclinical hypothyroidism, 20% had overt hypothyroidism and 8.33% were having hyperthyroidism. The most common symptom in metabolic syndrome patients with hypothyroidism was lethargy/sleepiness followed by dry and coarse skin. The most common symptom in hyperthyroid patients was nervousness (100%) followed by sweating, heat intolerance and palpitation in 80% of the patients.
Keywords: Metabolic syndrome, subclinical hypothyroid, hypothyroid, hyperthyroid
Introduction
The metabolic syndrome is a constellation of clinical and metabolic abnormalities including abdominal obesity, hypertension, dyslipidemia and impaired fasting glucose or impaired glucose tolerance. All these manifestations are surrogate markers of insulin resistance which is the crux abnormality associated with metabolic syndrome. Thyroid hormones markedly stimulate the basic metabolic rate and the metabolism of carbohydrate, lipids and proteins. This hormone appears to serve as a general pacemaker accelerating metabolic process and may be associated with metabolic syndrome. It also plays an important role in the development of the reproductive system. As metabolic syndrome and thyroid dysfunction (subclinical or overt hypothyroidism and hyperthyroidism) are independent risk factors for cardiovascular disease, it is possible that patients suffering from both these disease entities may have a compounded risk.
Aims and Objectives
The aim of this study was to determine the prevalence, symptomatology of thyroid dysfunction and fine needle aspiration cytology (FNAC) findings of thyroid in the patients having metabolic syndrome.
Material and Methods
In our study, 60 patients of metabolic syndrome without liver disease (viral, alcoholic, drug, autoimmune, etc.), chronic renal disease, pancreatitis and pregnancy were studied. Their clinical (age, sex, family history and blood pressure), biochemical (thyroid-stimulating hormone [TSH], free thyroxine [FT4], lipid profile, blood sugar) and thyroid FNAC profiles were studied. According to the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) at least three of the following criteria should be present to diagnose metabolic syndrome:
- Elevated waist circumference: Men - ≥90 cm for Indians, Women - ≥80 cm for Indians.
- Elevated triglycerides: ≥150 mg/dL.
- Reduced HDL (“good”) cholesterol: Men - <40 mg/dL, Women - <50 mg/dL.
- Elevated blood pressure: ≥130/85 mmHg.
- Elevated fasting glucose: ≥110 mg/dL.
The thyroid hormone assays (FT4 and TSH) were done using enzyme-linked immunosorbent assay (ELISA), and fasting blood sugar, triglycerides and high-density lipoprotein cholesterol (HDL-C) were done enzymatically on Roche Automated Clinical Chemistry Analyzer.
Diagnosis of thyroid dysfunction was made by FT4 and TSH - Euthyroid: normal TSH and normal FT4; Subclinical hypothyroidism: high TSH and normal FT4; Hypothyroidism: high TSH and low FT4 and Hyperthyroidism: low TSH and high FT4.
Observations and results
Our study group consisted of 24 male (40%) and 36 (60%) female patients. Male-to-female ratio was 2:3. Majority of patients (40.0%) belonged to age group 40-49 years. Mean age of all the patients was 47.6 ± 7.5 years. The mean age of males and females was 49.6 ± 8.0 and 46.2 ± 7.1, respectively.
The prevalence of components of metabolic syndrome (Fig. 1) in men and women were, central obesity in 18 (75%) and 30 (83.3%) patients, respectively; low HDL-C in 12 (50%) and 28 (77.8%) patients, respectively; high
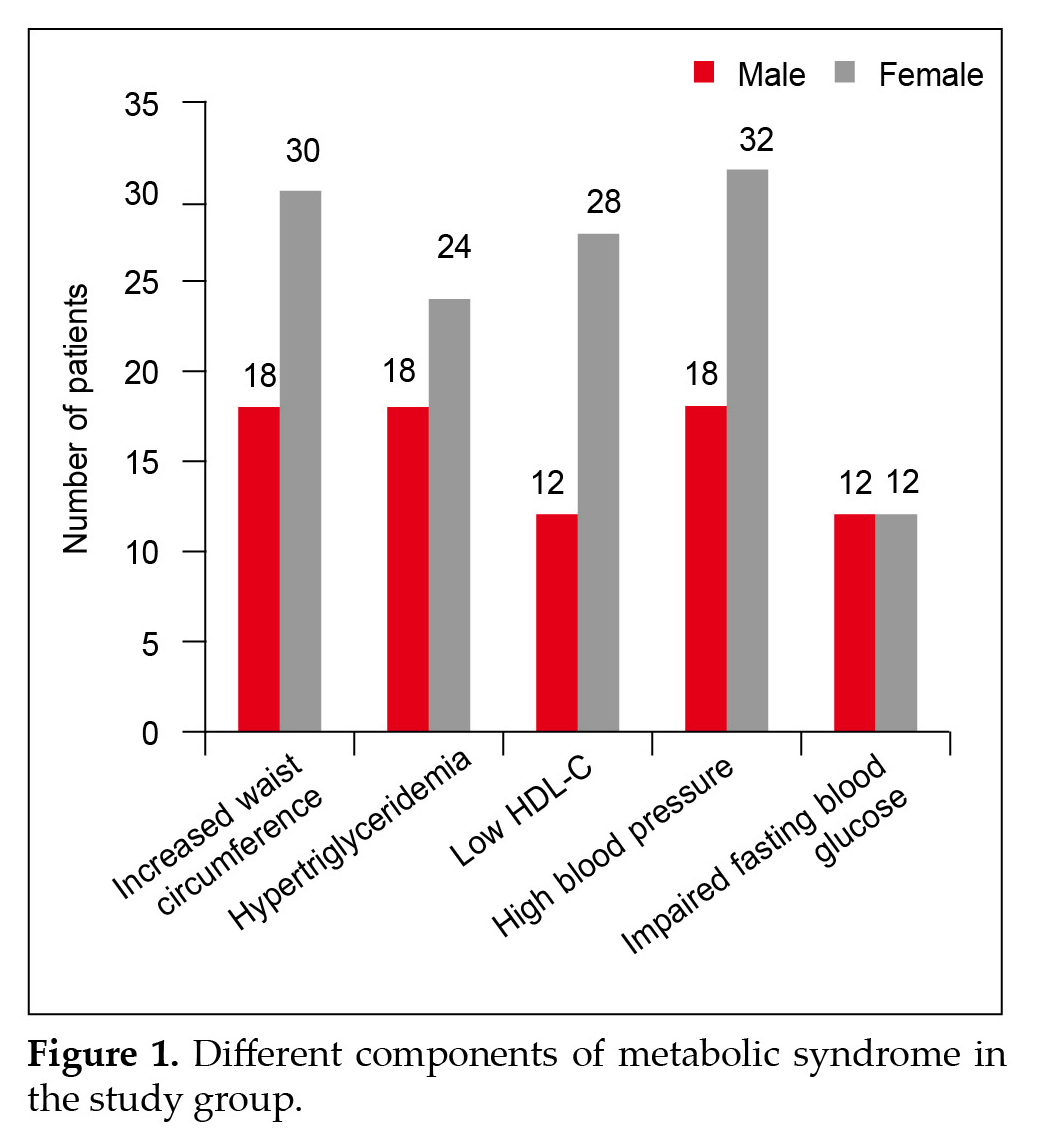
triglycerides in 18 (75%) and 24 (66.7%), respectively; impaired fasting glucose (>100 mg/dL) or diabetes in 12 (50.0%) and 12 (33.3%), respectively and elevated blood pressure in 18 (75%) men and 32 (88.9%) women.
Out of 60 patients of metabolic syndrome (Fig. 2), 30 patients (50%) were euthyroid, 13 patients (21.66%) had subclinical hypothyroid and 12 patients (20%) had overt hypothyroid while 5 patients (8.33%) had hyperthyroid.
The most common symptom (Table 1) in both subclinical and overt hypothyroid patients was (77.77%)
|
Table 1. Prevalence of Symptomatology of Hypothyroidism in the Study Group
|
|
Symptoms
|
Male
(n = 4)
|
|
Female
(n = 14)
|
|
Total
(n = 18)
|
|
No.
|
%
|
No.
|
%
|
No.
|
%
|
|
Lethargy/Sleepiness
|
3
|
75
|
11
|
78.57
|
14
|
77.77
|
|
Dry and coarse skin
|
3
|
75
|
10
|
71.42
|
13
|
72.22
|
|
Cold intolerance
|
2
|
50
|
10
|
71.42
|
12
|
66.66
|
|
Puffiness of face
|
2
|
50
|
10
|
71.42
|
12
|
66.66
|
|
Body aches
|
2
|
50
|
8
|
57.14
|
10
|
55.55
|
|
Weight gain
|
2
|
50
|
7
|
50
|
9
|
50
|
|
Constipation
|
2
|
50
|
9
|
64.28
|
11
|
61.11
|
|
Depression
|
2
|
50
|
8
|
57.14
|
10
|
55.55
|
|
Paresthesia
|
2
|
50
|
6
|
42.85
|
8
|
44.44
|
|
Menorrhagia
|
-
|
-
|
5
|
35.71
|
5
|
27.77
|
|
Thyroid gland size enlarged
|
1
|
25
|
5
|
35.71
|
6
|
33.33
|
|
Hair loss
|
1
|
25
|
4
|
28.57
|
5
|
27.77
|
| |
|
|
|
|
|
|
|
|
|
Table 2. Prevalence of Symptomatology of Hyperthyroidism in the Study Group
|
|
Symptoms and signs
|
Male
(n = 2)
|
|
Female
(n = 3)
|
|
Total
(n = 5)
|
|
No.
|
%
|
No.
|
%
|
No.
|
%
|
|
Nervousness
|
2
|
100
|
3
|
100
|
5
|
100
|
|
Sweating
|
2
|
100
|
2
|
66.66
|
4
|
80
|
|
Hypersensitivity to heat
|
1
|
50
|
3
|
100
|
4
|
80
|
|
Palpitation/Increased heart rate
|
2
|
100
|
2
|
66.66
|
4
|
80
|
|
Fatigue
|
1
|
50
|
2
|
66.66
|
3
|
60
|
|
Goiter
|
1
|
50
|
2
|
66.66
|
3
|
60
|
|
Hyperdefecation
|
1
|
50
|
1
|
33.33
|
2
|
40
|
|
Weight loss
|
1
|
50
|
2
|
66.66
|
3
|
60
|
| |
|
|
|
|
|
|
|
|
lethargy (sleepiness) followed by dry and coarse skin (72.22%), cold intolerance (66.66%), puffiness of face (66.66%), constipation (61.11%), depression (55.55%) and body aches (55.55%). Weight gain was seen in 50% and paresthesia in 44.44% hypothyroid patients. Thyroid gland size was enlarged in (33.33%) 6 patients. Five hypothyroid females (35.71%) had menorrhagia. Hair loss was present in 5 patients (27.77%).
The total number of hyperthyroid patients was 5 in the study. The commonest symptom (Table 2) was nervousness (100%) in our patients. Other symptoms like sweating (80%), hypersensitivity to heat (80%) and palpitation (80%) were also common in these patients. Fatigue, weight loss and enlarged thyroid (goiter) were present in 3 patients (60%). One male and 1 female hyperthyroid patient had hyperdefecation.
Twelve thyroid dysfunction patients with metabolic syndrome underwent FNAC of thyroid gland. Out of 12 patients, 8 patients (66.66%) had normal cytological findings. Two (1 subclinical hypothyroid and 1 overt hypothyroid) patients had simple colloid goiter and 1 overt hypothyroid had nodular colloid goiter. One hyperthyroid patient with metabolic syndrome had nodular hyperplasia of thyroid gland.
Discussion
In our study, out of 60 patients of metabolic syndrome, 30 patients (50%) were euthyroid, 13 patients (21.66%) had subclinical hypothyroid and 12 patients (30%) had overt hypothyroid. Five patients (8.33%) of metabolic syndrome had hyperthyroidism. A cross-sectional study from South India by Shantha et al has shown prevalence of subclinical hypothyroidism as 21.9% and overt hypothyroidism in 7.4% cases of metabolic syndrome.
The female-to-male ratio in our study was 2.25:1 in subclinical hypothyroidism and 2:1 in overt hypothyroidism patients. The female-to-male ratio in hypothyroidism ranges from 2:1 to 8:1 in various epidemiological surveys. Some surveys indicate hypothyroidism to be more prevalent in elderly population, reaching as high as 20%. Shrestha et al observed the association of metabolic syndrome in 21, 5 and 6 cases in 48 euthyroid, 24 hyperthyroid and 28 hyporthyroid groups, respectively.
The commonest symptom in hypothyroid patients was lethargy (77.77%). This was consistent with case-control study by Khurram et al in which 67.9% cases had lethargy. In our study too, dry and coarse skin was mentioned by 72.22% of patients like 70-79% cases in another study. Similarly, cold intolerance, that was found in 89% of patients in one series and 93% of another series, was prevalent in 66.66% of our cases, which is quite comparable to the 58.25% in Watanakunakorn’s. Five out of 14 (35.71%) females had menorrhagia as in the study by Khurram et al.
In a cohort study by Scott and Mussey, 28 women (56%) complained of menstrual disturbance, with the most common complaint being menorrhagia (occurring in 18 [36%] of the women). Other symptoms like body aches, weight gain, constipation, paresthesia, hair loss were similar to what has been described in various studies.
In our study, 66.66% patients had puffiness of face as compared to 63.3% in the study by Khurram et al, 79% in Lerman’s series and 67% in Watanakunakorn’s series.
Thyroid was enlarged in 6 hypothyroid patients (33.33%) as compared to 6.6% in the study by Samanta.
The most common symptom in hyperthyroid patients was nervousness (100%), followed by sweating (80%), hypersensitivity to heat (80%), palpitation (80%), weight loss (60%), fatigue (60%), hyperdefecation (40%) and goiter (60%), which was statistically comparable with the study by Trivalle et al.
Out of 12 patients who underwent FNAC of thyroid, 8 patients (66.66%) had normal cytological findings. Two (1 subclinical and 1 overt) hypothyroid patients had simple colloid goiter and 1 overt hypothyroid patients had nodular colloid goiter. One hyperthyroid patient with metabolic syndrome had nodular hyperplasia of thyroid gland.
In this study, we found that out of 60 patients of metabolic syndrome, 24 (40%) were male and 36 (60%)were female. Male-to-female ratio was 2:3 proving that disease was more dominant in females. Most of the patients of metabolic syndrome were belonging to age group 40-60 years. Mean age of males was 49.6 ± 8.0 years and mean age of female patients was 46.2 ± 7.1 years. Mean age of patients with metabolic syndrome in a study by Bacon and colleagues was 47 years and similarly another study also noted mean age of 54 years. About 23.3% of the patients met all the five diagnostic components of metabolic syndrome. Waist circumference was elevated in almost all (80%) the cases. Other components of metabolic syndrome were distributed in 50-70% of the patients.
Majority of male patients (45%) had waist circumference in range of 90-100 cm. Mean waist circumference of males was 97.9 ± 7.2 cm. Most of the female patients (40%) also had waist circumference in 90-100 cm range. Mean waist circumference of female patients was 97.8 ± 2.1 cm. In previous studies, mean waist circumference of males and females was 102 cm and 92 cm, respectively. About 62% of the patients had triglyceride level between 150 and 174 mg%. Only 14.3% had elevated triglyceride level more than 200 mg%. Mean triglyceride level of males was 160.1 ± 22.6 mg%.
Mean level of triglyceride in females was 162.7 ± 27.2 mg%. Liese et al noted hypertriglyceridemia in 50% of the cases. In previous studies, it was observed that mean triglyceride level in the patients of metabolic syndrome was 191.8 mg%.
About half of the patients (50.0%) had HDL level between 30 and 39 mg/dL. Mean HDL level of males was 40.8 ± 6.4 mg/dL. Female patients had mean HDL level 43.4 ± 7.5 mg/dL. There was a significant variation in mean HDL level between male and female patients. Similar studies in the past observed HDL abnormalities in 63.5% of the patients.
In our study, 40% patients of metabolic syndrome were diabetic. Only 8.3% patients had blood sugar in impaired glucose tolerance (IGT) range, 16.6% patients were newly diagnosed diabetics. Maximum number of patients (41.7%) were diabetic for duration more than 10 years. Matteoni et al also performed a similar study and found diabetes mellitus in 23% of cases.
In our study, 53% of patients with metabolic syndrome were hypertensive. In all, 25% were newly diagnosed hypertensives. About 37.5% had hypertension for duration more the 10 years. Kaplan and colleagues noted prevalence of hypertension in 58% patients of metabolic syndrome.
Conclusion
The present study concludes that 50% metabolic syndrome patients had thyroid dysfunction. Subclinical hypothyroidism was present in 21.66% and overt hypothyroidism 20% patients. Hyperthyroidism was observed in 8.33% of metabolic syndrome patients.
The most common symptom in metabolic syndrome patients with hypothyroidism was lethargy/sleepiness followed by dry and coarse skin.
The most common symptom in hyperthyroid metabolic syndrome patients was nervousness (100%) followed by sweating, heat intolerance and palpitation (80%). Thyroid dysfunction patients with metabolic syndrome presenting with goiter underwent FNAC of thyroid - 8 patients (66.66%) had normal cytological findings. Two (1 subclinical and 1 overt) hypothyroid patients had simple colloid goiter and 1 overt hypothyroid patient had nodular colloid goiter. One hyperthyroid patient with metabolic syndrome had nodular hyperplasia of thyroid gland. Metabolic syndrome and thyroid dysfunction are independent risk factors for cardiovascular disease. Their co-existence may even compound the risk of cardiovascular events. Hence, it is worthwhile to screen metabolic syndrome patients for thyroid dysfunction at the earliest for further decrease in cardiovascular events.
Suggested Reading
- Trivalle C, Doucet J, Chassagne P, Landrin I, Kadri N, Menard JF, et al. Differences in the signs and symptoms of hyperthyroidism in older and younger patients. J Am Geriatr Soc. 1996;44(1):50-3.
- Dillmann WH. Mechanism of action of thyroid Med Clin North Am. 1985;69(5):849-61.
- Shantha GP, Kumar AA, Jeyachandran V, Rajamanickam D, Rajkumar K, Salim S, et al. Association between primary hypothyroidism and metabolic syndrome and the role of C-reactive protein: a cross-sectional study from South India. Thyroid Res. 2009;2(1):2.
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486-97.
- Helfand M, Crapo LM. Screening for thyroid disease. Ann Intern Med. 1990;112(11):840-9.
- Tunbridge WM, Evered DC, Hall R, Appleton D, Brewis M, Clark F, et al. The spectrum of thyroid disease in a community: the Whickham survey. Clin Endocrinol (Oxf). 1977;7(6):481-93.
- Sawin CT, Chopra D, Azizi F, Mannix JE, Bacharach P. The aging thyroid. Increased prevalence of elevated serum thyrotropin levels in the elderly. JAMA. 1979;242(3):247-50.
- Shrestha S, Das BKL, Baral N, Chandra L. Association of metabolic syndrome and its components with thyroid dysfunction in females. Int J Diab Dev Ctries. 2007;27(1):24-6.
- Khurram IM, Choudhry KS, Muhammad K, Islam N. Clinical presentation of hypothyroidism: a case control analysis. J Ayub Med Coll Abbottabad. 2003;15(1):45-9.
- Lerman J, Means JH. The gastric secretion in exophthalmic goitre and myxoedema. J Clin Invest. 1932;11(1):167-82.
- Watanakunakorn C, Hodges RE, Evans TC. Myxedema; A study of 400 cases. Arch Intern Med. 1965;116:183-90.
- Scott JC Jr, Mussey E. Menstrual patterns in myxedema. Am J Obstet Gynecol. 1964;90:161-5.
- Samanta BB. Clinical profile of hypothyroidism. Available at: www.endocrineindia.com Clinical%20Profile%20Of%20 Hypothyroidism %20-PDF.pdf
- Bacon BR, Farahvash MJ, Janney CG, Neuschwander-Tetri BA. Nonalcoholic steatohepatitis: an expanded clinical entity. Gastroenterology. 1994;107(4):1103-9.
- DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. 1991;14(3):173-94.
- Liese AD, Mayer-Davis EJ, Haffner SM. Development of the multiple metabolic syndrome: an epidemiologic perspective. Epidemiol Rev. 1998;20(2):157-72.
- Alshkri M, Elmehdawi R. Metabolic syndrome among type-2 diabetic patients in Benghazi-Libya: a pilot study. Libyan J Med. 2008;3(4):177-80.
- Saely CH, Koch L, Schmid F, Marte T, Aczel S, Langer P, et al. Adult Treatment Panel III 2001 but not International Diabetes Federation 2005 criteria of the metabolic syndrome predict clinical cardiovascular events in subjects who underwent coronary angiography. Diabetes Care. 2006;29(4):901-7.
- Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116(6):1413-9.
- Kaplan NM. The deadly quartet. Upper-body obesity, glucose intolerance, hypertriglyceridemia, and hypertension. Arch Intern Med. 1989;149(7):1514-20.