Abstract
Background: Metabolic syndrome (Syndrome X/Insulin resistance syndrome) consists of central obesity, hypertriglyceridemia, low high-density lipoprotein (HDL) cholesterol, hyperglycemia and hypertension as its major features. All of them can be influenced by the functioning of a 20 g endocrine organ, the thyroid gland. Aims and objectives: To study the proposed association between metabolic syndrome and thyroid dysfunction. Material and methods: Hundred subjects aged more than 18 years, willing to participate in the study and fulfilling criteria of the National Cholesterol Education Program-Adult Treatment Panel III (NCEP-ATP III) for diagnosis of metabolic syndrome were included. Detailed clinical examination and laboratory investigations of all subjects were done. Risk factors were identified and analyzed by comparing the subjects with and without thyroid dysfunction. Results: Eighty-one out of 100 subjects with metabolic syndrome belonged to the age group between 41 and 70 years. Females comprised 60% of the total patient population with sedentary lifestyle as the major risk factor, whereas males comprising rest of the 40% had addictive behaviors as major risk factors. Observation of individual parameters under NCEP-ATP III showed that 57 patients fulfilled all 5 criteria, 34 patients fulfilled 4 and 9 patients fulfilled 3 criteria. Obesity and dyslipidemia were common among female subjects, whereas impaired glucose tolerance and hypertension were common among males. Thyroid dysfunction in the form of hypothyroidism was present in 30 subjects with females (23 patients) being the statistically significant population (p < 0.0001). Hypothyroidism was of subclinical type in 21 of these 30 subjects. None had hyperthyroidism. Left ventricular ejection fraction (mean ± SD) was lowered to 42.67 ± 6.53 from 49.07 ± 7.48 in presence of thyroid dysfunction in these subjects with metabolic syndrome (p < 0.0001). Conclusion: Metabolic syndrome and hypothyroidism (even subclinical) are both individual as well as combined risk factors for development of atherogenic dyslipidemia, diabetes mellitus and cardiovascular disease with elderly females comprising the high risk group.
Keywords: Metabolic syndrome, thyroid dysfunction, hypothyroidism
Introduction
Prevalence of both metabolic syndrome and thyroid dysfunction depend on features like age, sex, ethnicity and geographic factors.1 With increasing global industrialization and rising rates of obesity, prevalence of metabolic syndrome is expected to increase.
Metabolic syndrome and hypothyroidism share insulin resistance as the common pathophysiologic mechanism manifesting as obesity, dyslipidemia and hypertension.2,3 Study of association between these two disorders will help early identification of at risk group and initiation of treatment for thyroid dysfunction in individuals with metabolic syndrome.
Material and Methods
This was an observational and noninterventional study conducted in our Government Medical College and attached tertiary care hospital.
Study Group
Inclusion Criteria
Total of 100 subjects aged more than 18 years, willing to participate in the study and fulfilling criteria of the National Cholesterol Education Program-Adult Treatment Panel III (NCEP-ATP III) for diagnosis of metabolic syndrome were included (Table 1).
Exclusion Criteria
- Patients already diagnosed with thyroid dysfunction, thyroid malignancy.
- Pregnant females.
- Patients receiving drugs interfering with thyroid function.
Methods
- Detailed history of the patient including symptoms, past illness, occupation, lifestyle, familial and other comorbid illness obtained.
- General and systemic clinical examination of the patient was performed. Waist circumference and blood pressure (BP) were recorded.
- Following investigations were carried out:
- Serum fasting lipid profile
- Fasting blood sugar (FBS), postprandial blood sugar (PPBS), A1C
- Thyroid function tests - Serum thyroid-stimulating hormone (TSH), free T3, free T4 (Table 2)
- Complete blood count
- Renal and liver function tests
- Urine analysis
- 2D ECHO
- Chest radiograph
- Ultrasonography abdomen with kidney, ureter and bladder
- Electrocardiograph
- Fundus examination.
- Statistical analysis done for better understanding and to provide logical support to results.
Results
Patient population was largely comprised of middle-aged individuals with 81 out of 100 subjects with metabolic syndrome belonging to the age group between 41 and 70 years. Females comprised 60% of the total patient population with sedentary lifestyle as the major risk factor, whereas males comprising rest of the 40% had addictive behaviors as major risk factors (Table 3). Observation of individual parameters under NCEP-ATP III showed that 57 patients fulfilled all
5 criteria, 34 patients fulfilled 4 and 9 patients fulfilled 3 criteria. Sixty-six patients had waist circumference that satisfied the criteria for metabolic syndrome, whereas 73 patients had body mass index (BMI) of >25 kg/m2.
|
Tables 1. Clinical Identification of the Metabolic Syndrome: Any Three of the Following (NCEP-
ATP III Criteria)4
|
|
Risk factor
|
Defining level
|
|
Abdominal obesity
|
Waist circumference
|
|
Men
Women
|
>102 cm
>88 cm
|
|
Blood pressure
|
≥130/≥85 mmHg
|
|
Fasting glucose
|
≥110 mg/dL
|
|
Triglycerides
|
≥150 mg/dL
|
|
HDL cholesterol
Men
Women
|
<40 mg/dL
<50 mg/dL
|
|
Table 2. Thyroid Function Tests - Reference Values
|
|
Thyroid status
|
Serum TSH (µIU/mL)
|
Serum free T4
(ng/dL)
|
|
Eu
|
0.27-4.2
|
0.93-1.7
|
|
SCH
|
4.3-10
|
0.93-1.7
|
|
OH
|
>10
|
<0.93
|
Eu = Euthyroidism; SCH = Subclinical hypothyroidism;
OH = Overt hypothyroidism.
|
Table 3. Parameters of the Study Population
|
|
Parameters
|
Results
|
|
Age (years)
|
57.63 ± 10.58
|
|
Sex (M:F)
|
40:60
|
|
Waist circumference (cm)
Men
Women
|
101.43 ± 7.93
89.93 ± 9.04
|
|
Blood pressure (mmHg)
|
146.06/90.4
|
|
Fasting glucose (mg/dL)
|
133.71 ± 26.21
|
|
Total cholesterol (mg/dL)
|
233.45 ± 49.76
|
|
Serum triglycerides (mg/dL)
|
167.43 ± 20.53
|
|
Serum HDL (mg/dL)
Men
Women
|
37.18 ± 8.10
39.18 ± 7
|
|
Table 4. Association of Components of Metabolic Syndrome with Thyroid Function
|
|
Thyroid status
|
Waist circumference (cm)
|
Blood pressure (mmHg)
|
Fasting glucose
(mg/dL)
|
Serum Triglycerides
(mg/dL)
|
Serum HDL (mg/dL)
|
Total cholesterol (mg/dL)
|
|
Eu
|
95.91
|
142.8/84.3
|
123.36
|
161.97
|
39.16
|
214.03
|
|
SCH
|
91.67
|
146.6/88.6
|
130.38
|
172.29
|
37.33
|
262.67
|
|
OH
|
91.14
|
150.4/94.8
|
144.22
|
198.56
|
34.78
|
316.86
|
|
Table 5. Comparison of Parameters of Metabolic Syndrome with Thyroid Dysfunction Between Genders
|
|
Parameters
|
Male (Mean ± SD)
|
Female (Mean ± SD)
|
|
Waist circumference (cm)
|
91.58 ± 7.75
|
101.60 ± 7.84
|
|
Blood pressure (mmHg)
|
145.5/90.9 (mean)
|
148.4/91.7 (mean)
|
|
Fasting glucose (mg/dL)
|
132.69 ± 27.12
|
135.4 ± 24.98
|
|
Serum triglycerides (mg/dL)
|
167.60 ± 22.02
|
167.18 ± 18.32
|
|
Serum HDL (mg/dL)
|
39.33 ± 6.89
|
37.2 ± 8.86
|
|
Total cholesterol (mg/dL)
|
240.22 ± 45.66
|
226.55 ± 59.19
|
|
Serum TSH (µIU/mL)
|
7.62 ± 8.36
|
4.95 ± 3.64
|
|
Serum free T4 (ng/dL)
|
1.08 ± 0.26
|
1.16 ± 0.24
|
Sixty-six patients had hypertension and 33 had prehypertension. Only three patients were normotensive. Fifty patients had FBS between 100 and 125 mg/dL and 39 patients had frank type 2 diabetes. Eighty patients had triglyceride (TG) values >150 mg/dL and 4 among them had values >200 mg/dL. Thirty-one (78%) males had high-density lipoprotein (HDL) of <40 mg/dL and 56 (93%) females had HDL of <50 mg/dL. Total cholesterol and low-density lipoprotein (LDL) (not included in definition of metabolic syndrome) too were elevated among these patients. Obesity and dyslipidemia were common among female subjects attributable to sedentary lifestyle, whereas impaired glucose tolerance and hypertension were common among male subjects attributable to presence of addicting habits. Incidence of thyroid dysfunction was more common in patients satisfying more than three criteria for metabolic syndrome, in women with waist circumference >88 cm and in patients with diabetes mellitus (Table 4).
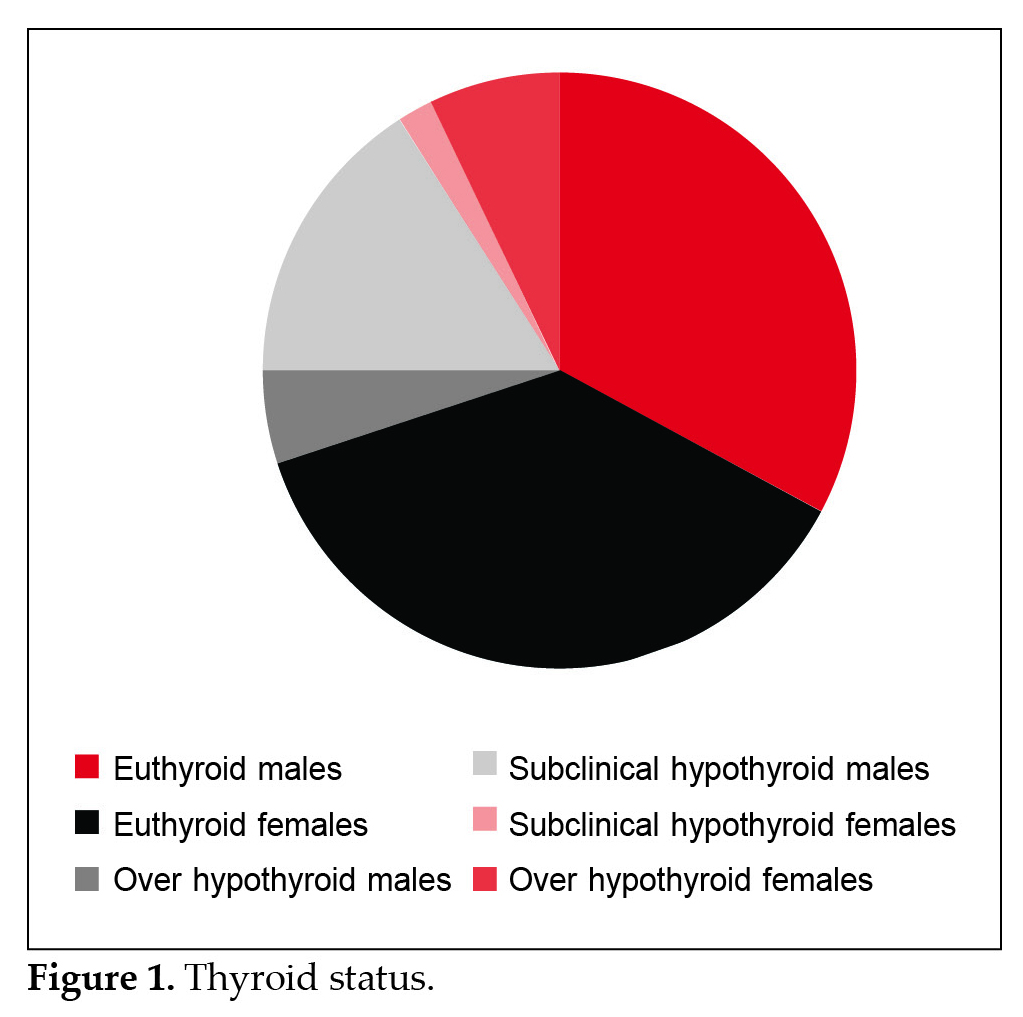
Prevalence of thyroid dysfunction in the form of hypothyroidism was statistically significant (p < 0.0001) in females than in males with 23 out of 60 female and only 7 out of 40 male subjects diagnosed with hypothyroidism (Table 5 and Fig. 1). Hypothyroidism was of subclinical type in 21 (16 females and 5 males) out of these 30 patients. None had hyperthyroidism. Left ventricular ejection fraction (LVEF) (mean ± SD) was lowered to 42.67 ± 6.53 from 49.07 ± 7.48 in presence of thyroid dysfunction in these subjects with metabolic syndrome (p < 0.0001).
Discussion
Metabolic syndrome is a cluster of cardiometabolic risk factors and hypothyroidism is an independent risk factor for cardiovascular disease.5-9 Both share insulin resistance as the central pathophysiologic mechanism. Insulin resistance favors lipolysis causing development of dyslipidemia and impaired glucose tolerance.10 Abdominal obesity further increases insulin resistance by producing inflammatory cytokines like tumor necrosis factor-? (TNF-?) and interleukin-6 (IL-6).11
Adiponectin released by adipose tissue enhances the action of insulin, but is deficient in obese persons.12,13 BMI >25 kg/m2 definitely forms a risk factor for atherogenic dyslipidemia and insulin resistance.14,15 Patients not having frank diabetes at present are prone to develop it in the future. Atherogenic dyslipidemia is reflected in the form of high serum TG, total cholesterol, LDL and low HDL. Studies suggest presence of linear correlation between dyslipidemia (high serum TG and cholesterol) and serum TSH values.16,17 Thyroid hormone affects tissue thermogenesis, erythropoiesis, lipid metabolism, systemic vascular resistance, blood volume, cardiac contractility, heart rate and cardiac output. Any thyroid dysfunction, therefore, alters cardiovascular dynamics significantly. Cardiac output increases 50-300% higher than in normal individuals in hyperthyroidism, whereas it may decrease by
30-50% in hypothyroidism. However, restoration of normal cardiovascular hemodynamics is possible with treatment of thyroid dysfunction.6-8
Present study reiterates that metabolic syndrome and hypothyroidism are both individual as well as combined risk factors for development of disease processes like cardiovascular disease and diabetes mellitus with elderly females comprising the high risk group.
Conclusion
Patients with metabolic syndrome and hypothyroidism (even subclinical) are prone to atherogenic dyslipidemia and cardiovascular events. Early thyroxine replacement can prevent cardiovascular events in these patients. Hence, we recommend routine screening for thyroid dysfunction in females with metabolic syndrome. However, theoretical benefits of thyroxine replacement in subclinical hypothyroidism is to be confirmed by future randomized trials.
References
- Delange F. The disorders induced by iodine deficiency. Thyroid. 1994;4(1):107-28.
- Roos A, Bakker SJ, Links TP, Gans RO, Wolffenbuttel BH.Thyroid function is associated with components of the metabolic syndrome in euthyroid subjects. J Clin Endocrinol Metab. 2007;92(2):491-6.
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486-97.
- National Institutes of Health, Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adults Treatment Panel III); executive summary. Publication No.01-3670. Bethesda: National Institutes of Health: 2001.
- Tkác I. Metabolic syndrome in relationship to type 2 diabetes and atherosclerosis. Diabetes Res Clin Pract. 2005;68 Suppl 1:S2-9.
- Klein I, Ojamaa K. Thyroid hormone and the cardiovascular system. N Engl J Med. 2001;344(7):501-9.
- Dillmann WH. Cellular action of thyroid hormone on the heart. Thyroid. 2002;12(6):447-52.
- Danzi S, Klein I. Thyroid hormone and the cardiovascular system. Minerva Endocrinol. 2004;29(3):139-50.
- Hak AE, Pols HA, Visser TJ, Drexhage HA, Hofman A,Witteman JC. Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: the Rotterdam Study. Ann Intern Med. 2000;132(4):270-8.
- Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988;37(12):1595-607.
- Ruan H, Lodish HF. Insulin resistance in adipose tissue: direct and indirect effects of tumor necrosis factor-alpha. Cytokine Growth Factor Rev. 2003;14(5):447-55.
- Kern PA, Di Gregorio GB, Lu T, Rassouli N, Ranganathan G.Adiponectin expression from human adipose tissue: relation to obesity, insulin resistance, and tumor necrosis factor-alpha expression. Diabetes. 2003;52(7):1779-85.
- Hara T, Fujiwara H, Shoji T, Mimura T, Nakao H, Fujimoto S.Decreased plasma adiponectin levels in young obese males. J Atheroscler Thromb. 2003;10(4):234-8.
- Grundy SM, Mok HY, Zech L, Steinberg D, Berman M. Transport of very low density lipoprotein triglycerides in varying degrees of obesity and hypertriglyceridemia. J Clin Invest. 1979;63(6):1274-83.
- Egusa G, Beltz WF, Grundy SM, Howard BV. Influence of obesity on the metabolism of apolipoprotein B in humans. J Clin Invest. 1985;76(2):596-603.
- Bauer DC, Ettinger B, Browner WS. Thyroid functions and serum lipids in older women: a population-based study. Am J Med. 1998;104(6):546-51.
- Asvold BO, Vatten LJ, Nilsen TI, Bjøro T. The association between TSH within the reference range and serum lipid concentrations in a population-based study. The HUNT Study. Eur J Endocrinol. 2007;156(2):181-6.